CT coronary angiography for assessing chest pain
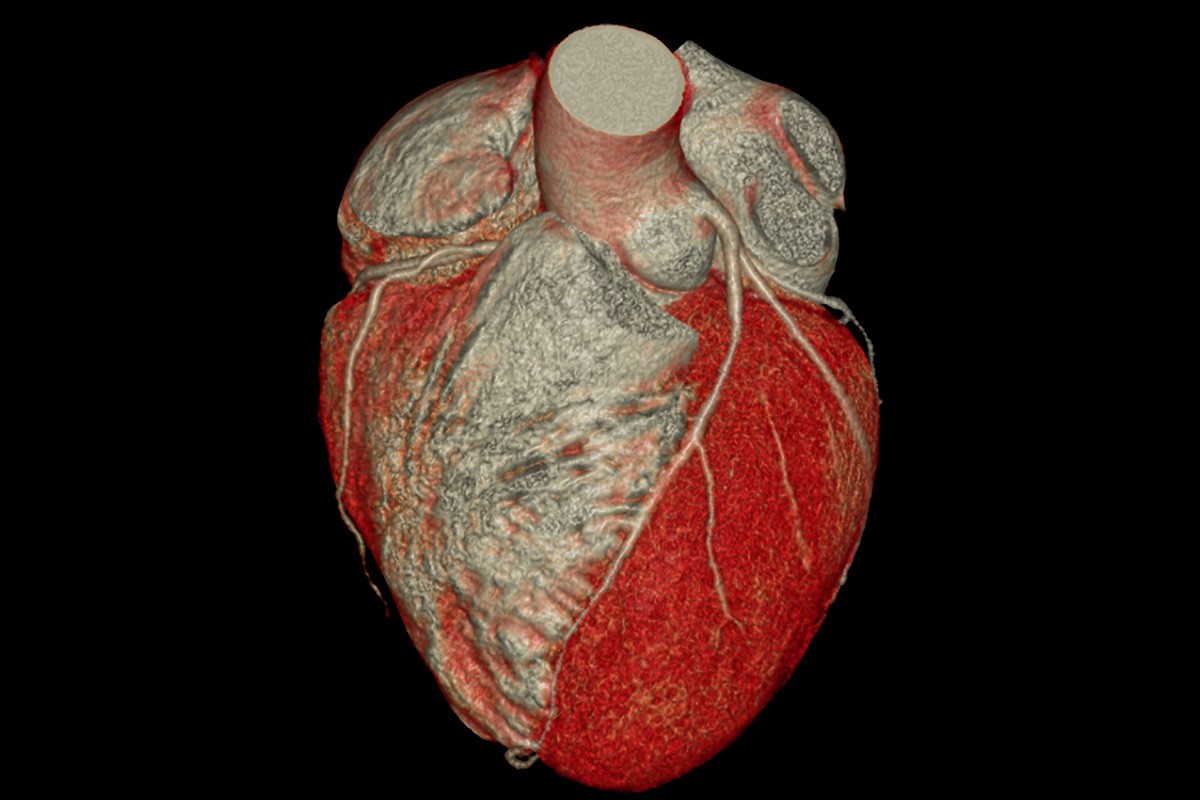
CT coronary angiography (CTCA) is a noninvasive diagnostic modality that comprehensively evaluates coronary arteries and atherosclerotic plaque within them. It has a very high sensitivity for detecting coronary artery disease. International guidelines increasingly support CTCA as a first-line diagnostic test for assessing stable chest pain in select patients. CTCA also plays an important role in cardiovascular risk stratification and guiding management of patients with chest pain, by determining whether preventive therapies or further investigations may be needed.
- Chest pain is a common presenting symptom for which obstructive coronary artery disease (CAD) should be excluded as a cause.
- CT coronary angiography (CTCA) noninvasively assesses coronary arteries and atherosclerotic plaque, including burden, luminal stenosis and composition.
- International guidelines increasingly support CTCA as a first-line diagnostic test in select low- to intermediate-risk patients with stable chest pain.
- CTCA detects plaque at all stages (from none to severe), thereby guiding use of preventive therapy and need for further testing.
- Due to its very high sensitivity, clinicians can confidently rule out CAD when CTCA shows normal coronary arteries.
- The accuracy of CTCA is affected by image quality, and knowledge of its limitations and contraindications is important when referring patients for the test.
- Recent advances in CTCA include use of artificial intelligence, high-risk plaque and perivascular inflammation analysis, and CT fractional flow reserve.
Chest pain is a common complaint in patients presenting to the emergency department and to GPs. Although the cause of chest pain is often not life-threatening, serious causes, such as obstructive coronary artery disease (CAD), need to be excluded.1 CAD is a leading cause of death in Australia, and early diagnosis and preventive therapies improve outcomes for patients.2 After excluding acute coronary syndrome, several noninvasive tests are available for diagnosing CAD, with the choice of test often depending on patient characteristics, cost, availability and expertise of local centres.3 The available tests include stress electrocardiography, stress echocardiography, myocardial perfusion imaging by nuclear single-photon emission CT and CT coronary angiography (CTCA). Recent international guidelines now support CTCA as a first-line diagnostic test in select patients with stable chest pain.4-6
Diagnosing coronary artery disease using CTCA
With the use of intravenous contrast, CTCA allows for a comprehensive three-dimensional assessment of coronary artery anatomy, luminal stenosis and plaque composition.7 Anomalous coronary arteries, a rarer cause of chest pain, can also be diagnosed by CTCA.8 CTCA has a very high sensitivity for detecting CAD and, because of its high negative predictive value, clinicians can confidently rule out CAD if CTCA shows normal coronary arteries.9-11
When CTCA shows severe luminal stenosis (i.e. 70% or greater), referral to a cardiologist is warranted for consideration of invasive coronary angiography. Patients with moderate stenosis (i.e. 50 to 69%) and symptoms are usually investigated further by functional (stress) testing to determine whether the lesion is causing significant ischaemia, before deciding whether invasive coronary angiography is needed. The Flowchart shows an approach to managing chest pain, and the Table summarises the factors favouring CTCA or stress testing as a first-line diagnostic test for chest pain.
Using CTCA to guide preventive therapies
The landmark Scottish Computed Tomography of the Heart (SCOT-HEART) trial showed that, in patients with stable chest pain presenting to outpatient clinics, use of CTCA increased diagnostic certainty and reduced the five-year risk of death from CAD events compared with standard care, which mostly involved exercise stress testing.12 CTCA led to a significant increase in the use of preventive pharmacotherapies, such as statins and aspirin, through detection of nonobstructive CAD.12 Detecting even mild CAD is important because nonobstructive plaque is also associated with increased cardiovascular risk, and its detection allows initiation of secondary preventive medical therapy to lower this risk.13,14
Studies have shown that overall plaque burden, rather than stenosis severity, is the main driver of future myocardial infarction.15 On the other hand, a CTCA scan showing normal coronary arteries is associated with very low cardiovascular risk, so unnecessary preventive pharmacotherapies can be ceased or avoided in the short term. The use of CTCA in assessing low- to intermediate-risk patients with chest pain and suspected CAD has been shown to be safe and cost-effective.3,16
Limitations of CTCA
The accuracy of CTCA is affected by image quality, which means that not all patients will be suitable for the test. To optimise image quality, patients are given medications (typically beta-blockers) to slow their heart rate to about 60 beats/minute, as well as glyceryl trinitrate to vasodilate the coronary arteries.17 Therefore, CTCA may not be suitable for patients whose heart rate cannot be adequately controlled, such as those with tachyarrhythmias or atrial fibrillation. Furthermore, because of the requirement for intravenous contrast, severe contrast hypersensitivity and significant renal impairment (estimated glomerular filtration rate of 30 mL/min/1.73 m2 or lower) are contraindications to CTCA.17 Significant coronary artery calcification or coronary artery stents can cause blooming artefacts, which also reduce diagnostic accuracy.17 Alternative diagnostic modalities may therefore be needed for some patients.
Medicare reimbursement for CTCA is only available via specialist referral, so GPs will generally need to refer patients to a cardiologist to access the test. However, there has been an increase in the availability of rapid access chest pain clinics, which can provide more efficient investigation and management of patients with chest pain and where CTCA may be more easily accessible.
Finally, it is important to note that noncontrast coronary artery calcium scoring alone (without imaging of the coronary lumen) is insufficient for excluding coronary stenosis in symptomatic patients presenting with chest pain.
Recent advances in CTCA
Radiation exposure in CTCA has significantly decreased, with scans now being performed at doses less than 2 to 3 mSv.18,19 New software and artificial intelligence algorithms have been integrated into CT imaging and have shown increasing potential for optimising image acquisition and analysis. Assessment of plaque composition and morphology can give patients a more personalised risk assessment by adding unique prognostic information beyond percent luminal stenosis.20 High-risk ‘vulnerable’ plaque features on CTCA (including low attenuation, positive remodelling, spotty calcification and the ‘napkin ring’ sign) have been shown to correlate with increased risk of future CAD events.21-23 The perivascular fat attenuation index is a measure of coronary artery inflammation on CTCA that also predicts future CAD events; this biomarker technology is TGA approved for use in Australia.24 CT-derived fractional flow reserve (CT-FFR) uses computational fluid dynamics and allows CTCA to become both an anatomical test and a functional test for lesion-specific ischaemia. However, CT-FFR is not yet widely available in Australia.
Conclusion
CTCA is a noninvasive diagnostic modality that can be considered as a first-line test for assessing chest pain in select low- to intermediate-risk patients, according to international guidelines. CTCA offers advantages over stress testing in detecting CAD and in identifying patients who require medical therapy or further functional testing. The ability to assess the burden, location and severity of coronary atherosclerotic plaque can guide decision making and improve patient outcomes. Advances in CTCA have the potential to allow for more personalised risk assessment and to change patient management. Although CTCA remains largely a specialist referral test in Australia, rapid access chest pain clinics may provide a streamlined pathway for patients to access this as a first-line test. CT
COMPETING INTERESTS: None.