What’s my heart disease risk, doctor? A practical guide to the 2023 Australian CVD risk guideline
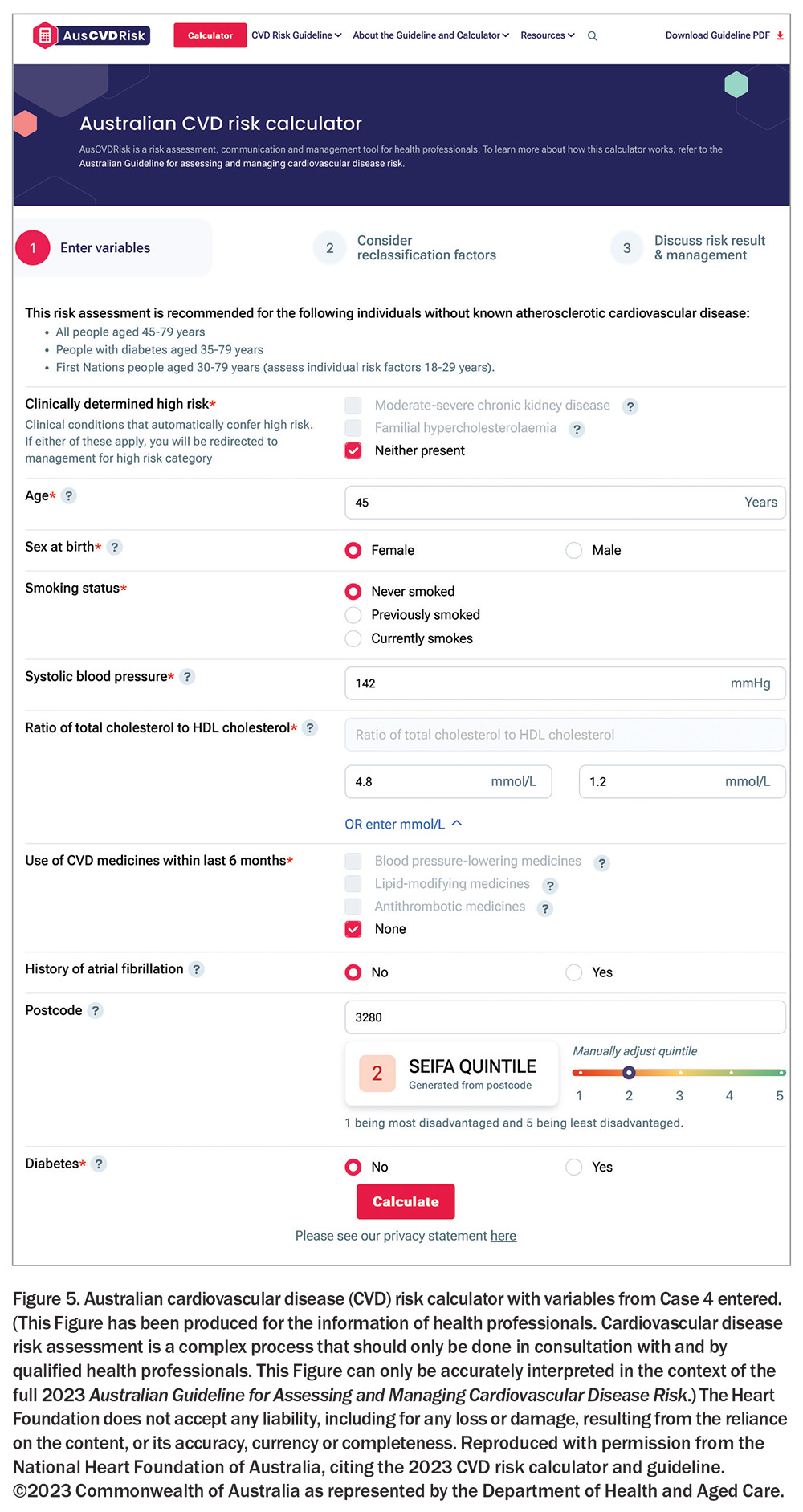
The 2023 Australian Guideline for Assessing and Managing Cardiovascular Disease Risk with its new calculator takes a more holistic approach to estimating risk and patient classification. Apart from the classic risk factors of age, sex, smoking status, diabetes, blood pressure (BP) and lipids, it also considers the use of BP-lowering and lipid-modifying medicines, a diagnosis of atrial fibrillation and postcode as a surrogate for socioeconomic status.
- The 2023 Australian Guideline for Assessing and Managing Cardiovascular Disease Risk recommends cardiovascular disease (CVD) risk assessment for people aged 45 to 79 years, for people with diabetes from the age of 35 years, and for First Nations people from the age of 30 years. Individual CVD risk factors should be assessed in First Nations people aged 18 to 29 years.
- The new Australian CVD risk (Aus CVD Risk) calculator includes optional risk factors that were not part of the previous Framingham-based equation, including a diagnosis of atrial fibrillation and socioeconomic status through a surrogate of residency postcode. It also allows for improved CVD risk estimation in people with type 2 diabetes, factoring in glycated haemoglobin, time since diagnosis of diabetes (measured in years), urinary albumin-to-creatinine ratio, estimated glomerular filtration rate, body mass index and the use of insulin in the previous six months.
- Risk categories have been redefined in the new Aus CVD Risk calculator, providing a more accurate risk prediction than the previous calculator. Reclassification factors have been introduced to allow for improved individual management.
- Relevant decision aids should be used to support effective risk communication and enable informed decisions about reducing CVD risk.
- Managing CVD risk should always include advice on appropriate healthy lifestyle and behaviours, with or without blood pressure-lowering and lipid-modifying pharmacotherapy.
‘What’s my heart disease risk, doctor?’ If only our patients started a consultation with this request. In reality, it is often the doctor who needs to raise this issue prompted by their knowledge of the patient’s age, sex, cultural background and cardiovascular disease (CVD) risk factors. Historically, doctors approached this by monitoring risk factors such as blood pressure (BP) and cholesterol and giving a BP- or lipid-lowering medication to a patient who crossed an arbitrary individual risk-factor threshold. Over a decade ago, peak bodies recommended moving from this approach to a more holistic one, leading to formal calculation of a validated risk score that best identifies those most likely to have a major adverse cardiovascular event (MACE) in the intermediate future and, therefore, who to treat.1 Subsequent research showed that these guidelines were not universally observed, with 60% of high-risk individuals not receiving lipid- and BP-lowering therapy as recommended.2 The passage of time and the need to reinvigorate this approach led to the development of a new risk calculator and the publication of the 2023 Australian Guideline for Assessing and Managing Cardiovascular Disease Risk.3
Why the need for a new calculator and why this one?
The best performed algorithms are those based on local, contemporary populations. With the decline in the age-standardised rates of MACE, the Framingham-based risk equation used in the 2012 guideline’s CVD risk calculator, while maintaining reliable ranking, had drifted into overestimating risk in the general population and continued to underestimate risk in other groups, including First Nations people.4
The Guideline Expert Steering Group sought to identify a suitable local dataset to develop a new calculator, but unfortunately one did not exist (for Steering Group members, refer to Appendix 2 of the Guideline3). Of the international equations considered, the PREDICT-1° equation, which was developed using datasets from a large contemporary New Zealand primary care cohort study, was found to be best suited for adaptation to Australia.5
Any calculator for practical use needs to balance inputs with outputs – i.e. how many variables are needed to enter before it does not add substantially to the risk estimate and patient classification. The ‘classic six’ of age, sex, smoking status (current/ex/never), diabetes, BP and lipid levels provides most of what is needed. The new Australian CVD risk (Aus CVD Risk) calculator includes optional risk factors such as a diagnosis of atrial fibrillation (AF) and postcode, which were not part of the previous Framingham-based calculator. AF is an important individual risk factor for stroke, and postcode is a surrogate measure of socioeconomic status. The postcode can be manually adjusted at the discretion of the clinician to better reflect an individual’s socioeconomic status.
The previous calculator was for patients who were treatment-naïve, so the addition of a variable that accounts for treatment (use of BP-lowering, lipid-modifying and antithrombotic medicines) widens the Aus CVD Risk calculator’s utility.
The Aus CVD Risk calculator also allows improved CVD risk estimation in people with type 2 diabetes, with optional additional inputs such as years since diabetes diagnosis, glycated haemoglobin level, urine albumin-to-creatinine ratio, estimated glomerular filtration rate, body mass index and the use of insulin.
Who should have their CVD risk estimated?
Risk estimation is recommended for people without known CVD. People with overt CVD or with moderate-to-severe chronic kidney disease and familial hypercholesterolaemia should be automatically managed as having a high CVD risk.
The Aus CVD Risk calculator allows an expanded age range for estimating risk: all people aged 45 to 79 years, people with diabetes aged 35 to 79 years and First Nations people aged 30 to 79 years (assessing individual risk factors for those aged 18 to 29 years).
Risk categories have been redefined according to the new Aus CVD Risk calculator, which provides a more accurate risk prediction than the previous calculator:
- high (≥10% risk over five years)
- intermediate (5 to <10% risk over five years)
- low (<5% risk over five years).
The calculator also allows reclassification of an individual, especially when the calculated risk is close to a risk category threshold. Reclassification can be upward or downward according to ethnicity or coronary artery calcium score, or upward with substantiated premature CVD family history, chronic kidney disease or personal severe mental illness.
Practical use of the Aus CVD Risk calculator
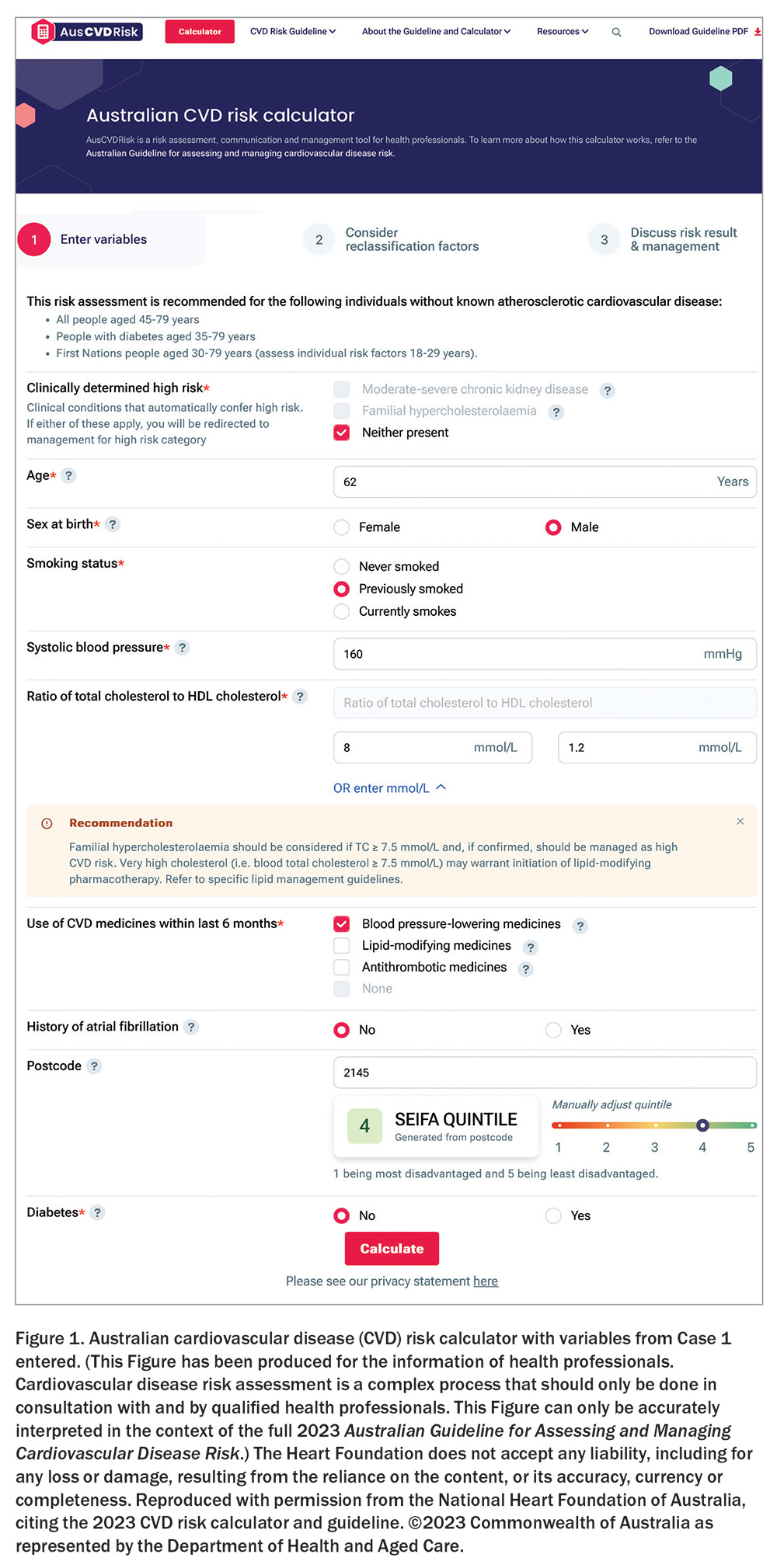
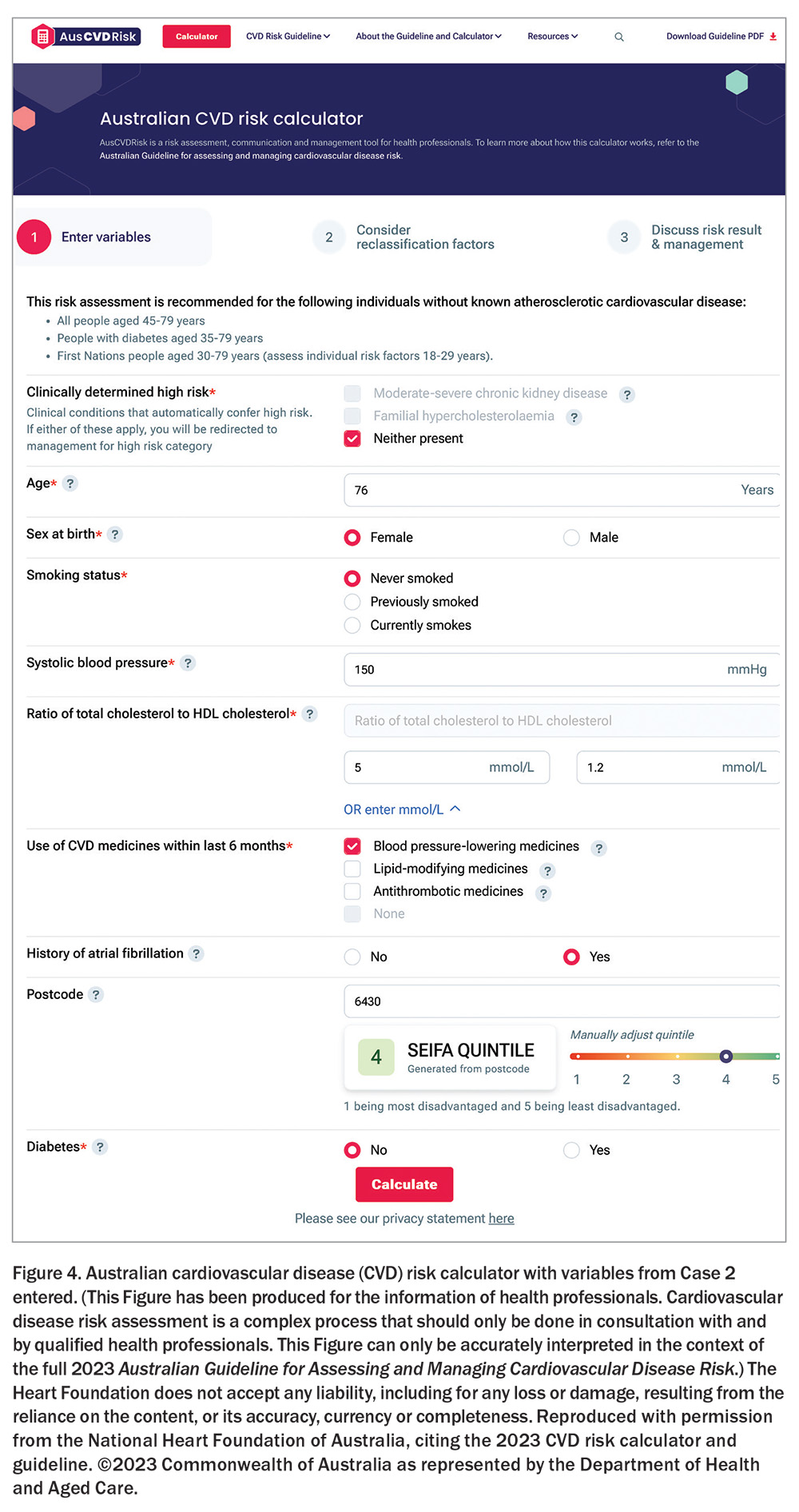
The following case vignettes illustrate how a patient can have a risk estimation calculated and communicated for shared decision-making on therapies and behavioural modification. Figures 1 to 5 can be recreated by entering the variables from the cases into the Aus CVD Risk calculator. The Aus CVD Risk calculator can be accessed via the website cvdcheck.org.au.3 Work is underway to integrate it into clinical software.
Case 1
Mr Kevin Jones is a 62-year-old man of Caucasian background, working in a job in which he is on his feet all day. He is an ex-smoker with a 40 pack-year history and lives in the Sydney suburb of South Wentworthville (Socio-Economic Indexes for Areas [SEIFA] quintile of 4, with 1 being the most disadvantaged and 5 being the least disadvantaged). His fasting blood tests indicate a total cholesterol level of 8 mmol/L, with an HDL cholesterol level of 1.2 mmol/L and a blood glucose and renal function in the normal range. His BP is 160/85 mmHg despite having started BP-lowering therapy three weeks previously (Figure 1). His mother had a fatal myocardial infarction before age 60 years.
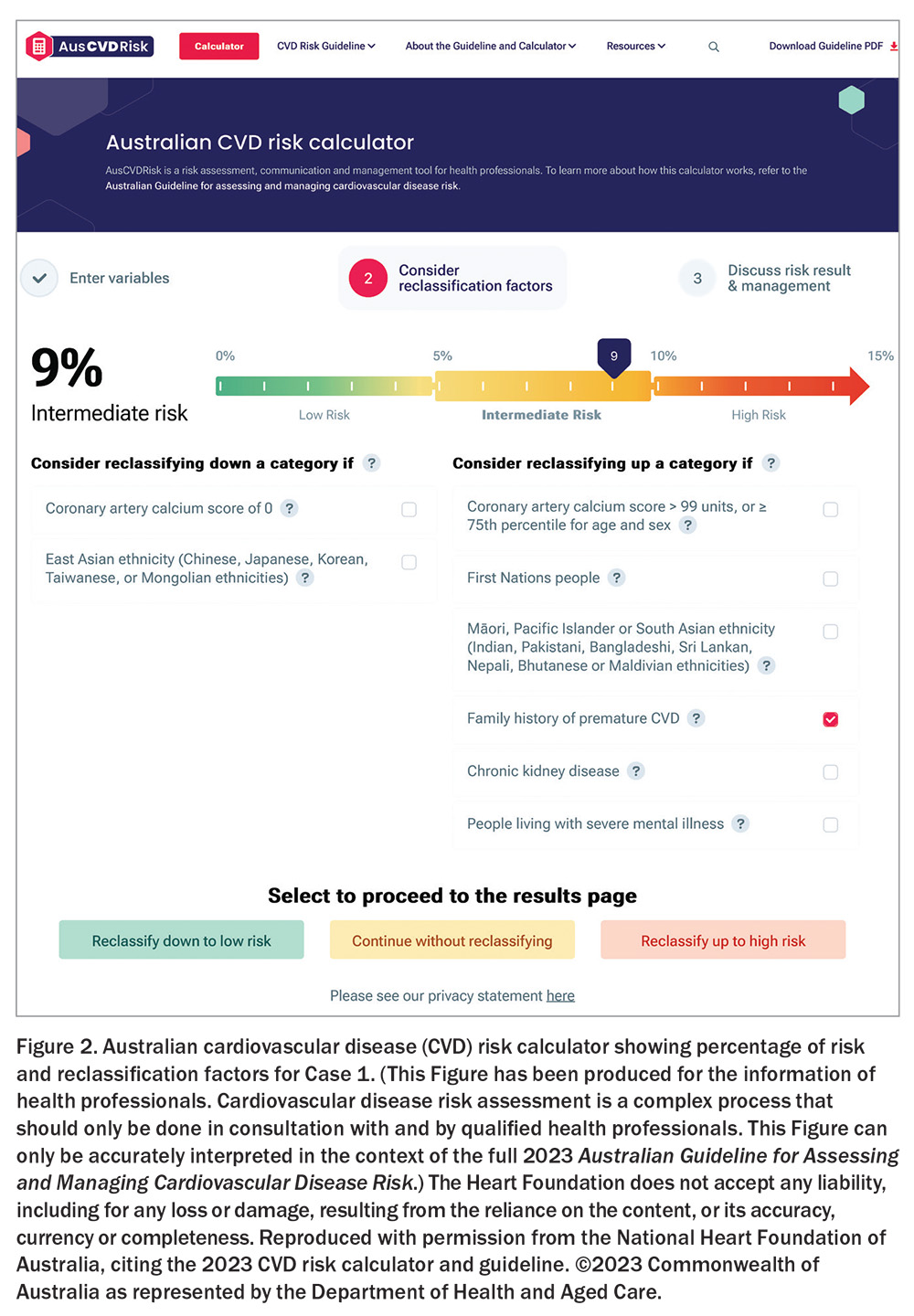
Mr Jones should be considered for possible familial hypercholesterolaemia through a more extensive family history and physical examination with a Dutch Lipid Clinical Network Score.6,7 Only when this is excluded should a formal risk score be generated. So reassured, after entering his risk factors into the calculator, he is estimated to have a 9% risk of having a CVD adverse event in the next five years (Figure 2).
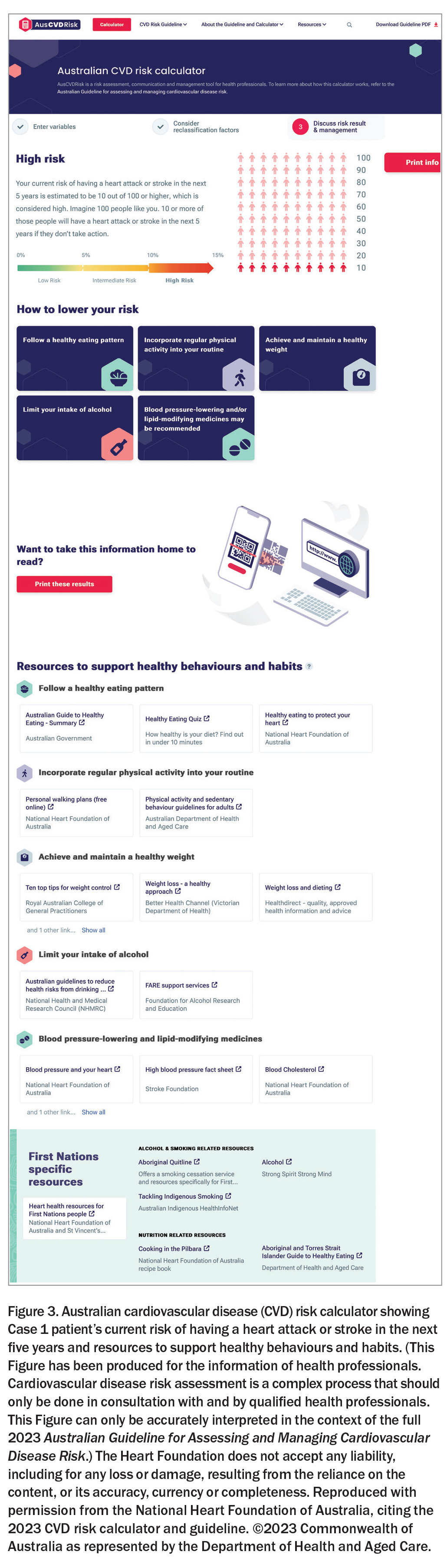
This is an intermediate risk close to a threshold, but Mr Jones has a reclassification factor of a family history so could be reclassified as high risk or further investigated with a calcium coronary score or computed tomography coronary angiogram. It is reasonable to conclude that he needs further BP-lowering therapy and the introduction of lipid-lowering therapy. The risk needs to be communicated to him (either as a percentage or as a frequency – e.g. 10% or ‘10 out of 100 people like you will have a heart attack or stroke in the next five years’), as do the benefits of BP- and lipid-lowering therapy and recommended behavioural changes. Appropriate materials to support healthy behaviours and habits can be printed for the patient to take with him (Figure 3).
Case 2
Mrs Gloria Williams is a 76-year-old nonsmoking woman of Caucasian background who lives on her own in the Western Australian Goldfields town of Kalgoorlie (SEIFA quintile 4). She is quite active, working two days a week in a shop, swimming in summer and walking in winter. Her fasting blood tests indicate a total cholesterol level of 5 mmol/L, with an HDL cholesterol level of 1.2 mmol/L and a blood glucose level and renal function in the normal range. Her BP is 150/85 mmHg on BP-lowering therapy. She has a history of paroxysmal AF, although she is not in AF now, and not keen to take oral anticoagulants (Figure 4).
On entering these data into the Aus CVD Risk calculator, Mrs Williams has a 15% (high) risk of a CVD event in the next five years. Given her good behavioural profile, the risk-reduction strategy is limited to pharmacotherapy (lipid-lowering and further BP-lowering therapy and revisiting her reluctance to take anticoagulants given her high stroke risk).
Case 3
Ms Seema Sharma is a 56-year-old woman originally from Goa, India, with longstanding diabetes (15 years) who presented for routine medications after a recent hospitalisation for an acute coronary syndrome (ACS). Her medical records were updated, including medication changes. She was asked about her symptoms, and an examination was conducted. She was encouraged to attend her cardiac rehabilitation sessions. Ms Sharma has overt coronary artery disease and, therefore, does not need a risk calculation and her CVD risk factors should be treated vigorously. However, this is a teaching moment, and a critical event audit can be undertaken to identify if the ACS event could have been avoided.
Ms Sharma’s attendance before her hospitalisation noted that she was a nonsmoker, her glycated haemoglobin level was 7.4%, BP 144/84 mmHg (on one BP-lowering therapy), fasting total cholesterol level 6.4 mmol/L, HDL cholesterol level 0.9 mmol/L and body mass index 28.1 kg/m2 and she had normal renal function. Her risk score pre-event was 9% and given this level and her ethnicity warranted reclassification to high risk. Thus, additional BP-lowering and lipid-modifying therapy would have been recommended if this CVD risk estimation had been done and perhaps the ACS event avoided or delayed.
Case 4
Ms Su Lee is a 45-year-old shop assistant of Chinese descent living in the Victorian coastal town of Warrnambool (SEIFA quintile 2). Her clinic and home BP are persistently in the low 140 mmHg range, and she has previously been screened for secondary causes of high BP and CVD risk factors. Her BP today is 142/85 mmHg. She is a nonsmoker and has normal fasting glucose level, a total cholesterol level of 4.8 mmol/L and an HDL cholesterol level of 1.2 mmol/L (Figure 5). A risk calculation returns a score of 1%.
The guideline recommendation would not be to initiate BP-lowering or lipid-lowering medication as the effectiveness of medication is predicated on an individual’s absolute risk and, therefore, those at lowest risk have the least benefit from them. Investigation of her antecedent adverse risk factors for high BP reveals her regular consumption of a two-litre cask of white wine over two days and a high sodium intake in her mainly Chinese diet. Patient education from a dietitian on alcohol moderation and salt reduction is required and brings health benefits beyond the simple lowering of BP with medication.
Conclusion
Our patients’ risk of developing overt CVD depends on the combined effect of multiple risk factors. Risk assessment remains fundamental to the primary prevention of CVD. It encourages modification of early CVD risk factors, helps target pharmacotherapy to those who will benefit most from it and informs clinical decision-making. CT
COMPETING INTERESTS: Professor Nelson has received a speaker’s fee from Medtronic post membership of the guideline committee. Professor Jennings is the Chief Medical Advisor of the National Heart Foundation of Australia (NHFA); NHFA, on behalf of the Australian Chronic Disease Prevention Alliance, received funding from the Australian Government Department of Health and Aged Care to develop the 2023 Australian Guideline for Assessing and Managing Cardiovascular Disease Risk and the Australian CVD Risk Calculator and to lead its implementation in general practice. He is Associate Editor of Hypertension, a journal of the American Heart Association. He is on the Advisory Board of SiSu Health, a past Member of the Global Vaccine Advisory Board, Sanofi Pasteur, and Senior Advisor to Sydney Health Partners.
Acknowledgement: The authors thank Tina Garcia, Senior Medical Writer at the National Heart Foundation of Australia, for editorial support in accordance with Good Publication Practice (GPP3) guidelines.
References
1. National Vascular Disease Prevention Alliance. Guidelines for the management of absolute cardiovascular disease risk. Canberra: NVDPA; 2012.
2. Banks E, Crouch SR, Korda RJ, et al. Absolute risk of cardiovascular disease events and blood pressure- and lipid-lowering therapy in Australia. Med J Aust 2016; 204: 320.
3. Australian Government Department of Health and Aged Care. Australian guideline for assessing and managing cardiovascular disease risk, 2023. Canberra: Commonwealth of Australia; 2023. Available online at: https://www.cvdcheck.org.au/ (accessed October 2024).
4. Brown S, Banks E, Woodward M, et al. Evidence supporting the choice of a new cardiovascular risk equation for Australia. Med J Aust 2023; 219: 173-186.
5. Australian Government Department of Health and Aged Care. How the calculator was developed. Available online at: https://www.cvdcheck.org.au/how-the-calculator-was-developed (accessed October 2024).
6. FH Australasia Network. Dutch Lipid Clinical Network Score (DLCNS) Online Calculator. Available online at: https://www.athero.org.au/fh/calculator/ (accessed October 2024).
7. Watts GF, Sullivan DR, Hare DL, et al. FH Australasia Network Consensus Working Group. Integrated guidance for enhancing the care of familial hypercholesterolaemia in Australia. Heart Lung Circ 2021; 30: 324-349.