Sinus pause and arrest
Articles in this section are inspired by, but not based on, real cases to illustrate the importance of knowledge about ECGs in relation to clinical situations in general practice. Management is not discussed in detail.
- Sinus pause is defined as a delayed impulse from the sinoatrial node of 2 or more seconds’ duration, as measured from the beginning of one P wave to the beginning of the next on the ECG trace.
- Sinus arrest is most appropriately used when there is a very prolonged flatline with syncope or cardiorespiratory arrest.
- Sinus pauses and arrest are part of the spectrum of sinus node dysfunction.
- Medications such as beta blockers, calcium channel blockers and digoxin may cause or contribute to sinus node bradycardia and sinus pauses and arrest.
- The most common cause of sinus pause or arrest in the absence of medications is idiopathic, typically age-related, degeneration and fibrosis of the sinoatrial nodal tissue.
- An implantable cardiac loop recorder or cardiac event recorder monitors the electrical activity of the heart continuously and can transmit to and alert the cardiologist if there is a significant abnormality. Some apps on smartphones, watches and tablets can perform similar functions.
Frank is an 83-year-old man who is well known to your practice. He is extremely health-focused and still walks 5 km daily. He is on metoprolol 25 mg twice daily and candesartan 16 mg in the morning for hypertension that he has had for 25 years. It has always been well controlled and Frank ensures this by measuring his blood pressure several times daily. His lipids are at target and he has normal glucose tolerance. Frank has never smoked. He had his first knee replacement three years ago and is now going to have his second done. He wants to have a full cardiac review before surgery and he is asymptomatic. He had a cardiac review previously with a cardiologist when he turned 80 years, before his first knee replacement, and at that time he had a normal stress echocardiogram and a low calcium artery score for his age.
Initially, Frank has blood tests and shows you an ECG strip recorded by a smartphone app.
Q1. What does the ECG strip show?
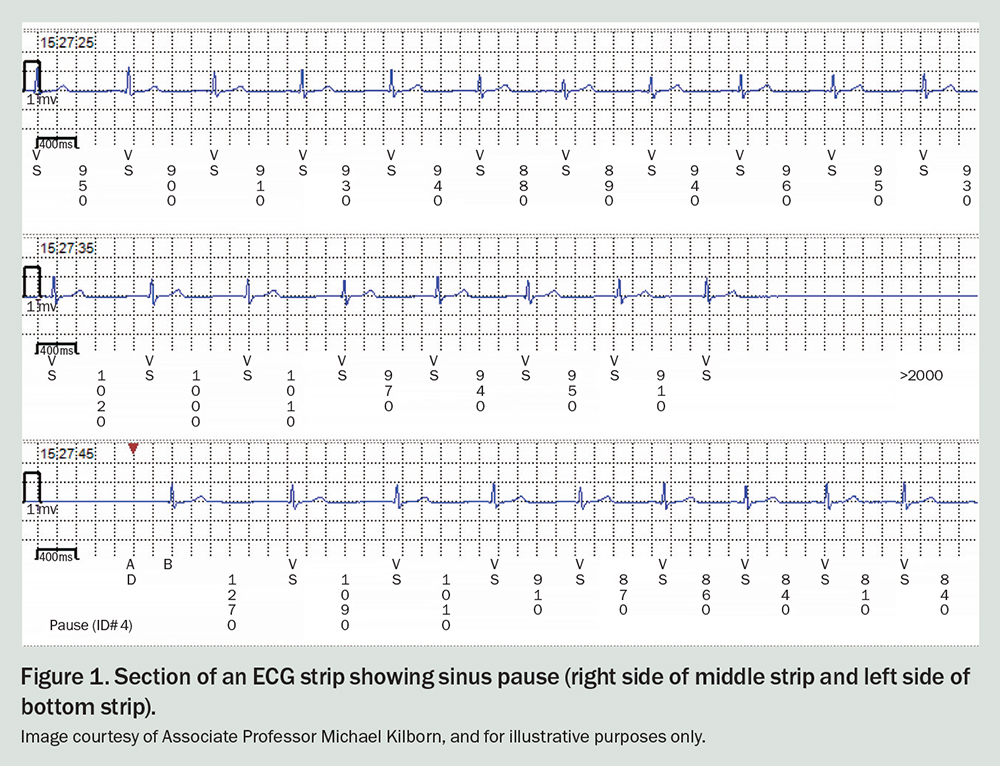
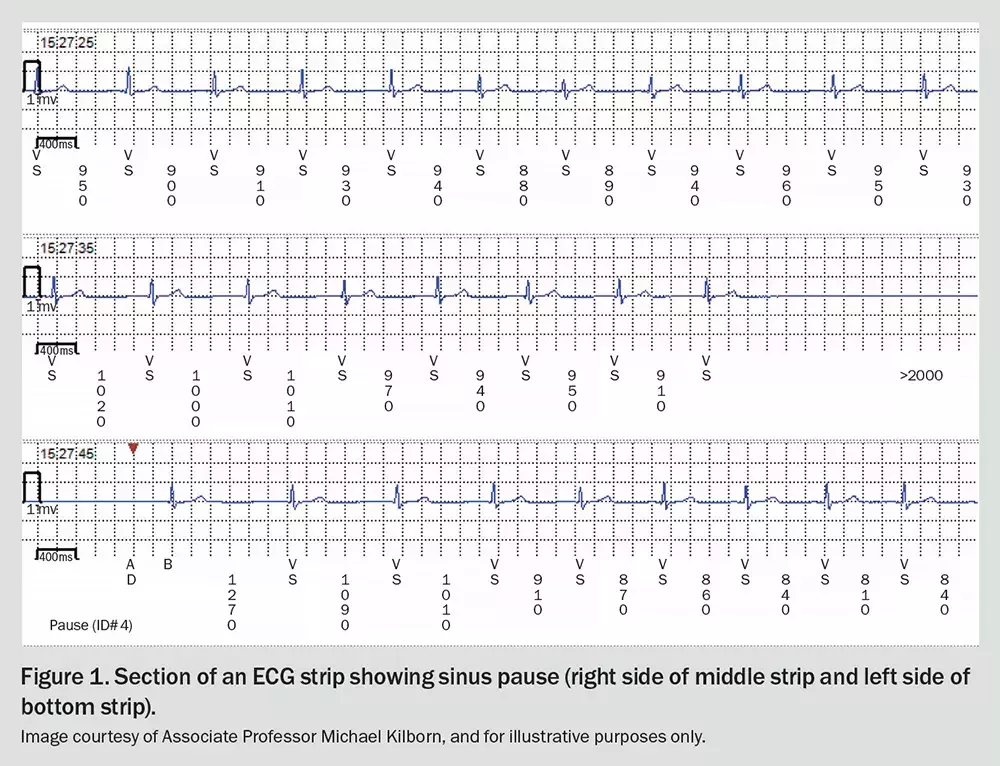
The ECG strip in Figure 1 shows a sinus pause of greater than 3 seconds. Apart from this, the strip is normal.
Q2. What is the definition and electrophysiological cause of sinus pause or arrest?
The terms sinus arrest and sinus pause are often used interchangeably when there is a delayed impulse from the sinus node over the range of 3 to 10 seconds. ‘Arrest’ is most appropriately used when there is a very prolonged ‘flatline’ with syncope or cardiorespiratory arrest.
The definition of a sinus pause or arrest is a delayed impulse from the sinoatrial node lasting 2 seconds or more (pause) or 3 seconds (arrest), as measured from the beginning of one P wave to the beginning of the next on the ECG trace. This is seen on the ECG as an absence of a P-wave or QRS complex for at least this duration.
Sinus pauses and arrest are part of the spectrum of sinus node dysfunction. This spectrum includes sinus bradycardia, sinus arrhythmia not related to respiration, tachy-brady syndrome (sick sinus syndrome), sinoatrial exit block (where the impulse does not travel further than the sinus node) and sinus arrest. Pauses are often seen after ectopic beats.
When sinus arrest occurs, ‘escape’ beats may occur until the sinoatrial node recovers. These may originate from areas in the atrial myocardium that possess pacemaker function, from cells adjacent to the atrioventricular (AV) node, or from the His-Purkinje network, which can depolarise at the rate of 20 to 40 beats per minute. They often appear to be a QRS complex with no preceding P wave. If the escape beats have a broad QRS complex they are called a ‘ventricular rhythm’.1
Q3. What are the causes of sinus pause and arrest?
Medications such as beta blockers, calcium channel blockers and digoxin may cause or contribute to sinus node bradycardia, sinus pauses and sinus arrest.
The most common cause in the absence of medications is idiopathic, typically age-related, degeneration and fibrosis of the sinoatrial nodal tissue. Hypothyroidism and hyperkalaemia should be excluded as causes. Other causes include myocardial ischaemia, cardiomyopathy, autonomic dysfunction, storage diseases of the myocardium (sarcoidosis and haemochromatosis) and congenital abnormalities of the electrical conduction system.
Q4. What is the differential diagnosis of sinus arrest?
AV block may appear to be sinus arrest if the P waves are low amplitude. Careful inspection of all leads will usually find P waves if they are present. Autonomic abnormalities affecting the sinus node may be the primary problem, as in vasovagal or neurocardiogenic syncope. Artefacts in ECG recordings must also be considered – clues may be absence of symptoms at the time of the recording and sharp discontinuities between the periods of flatlining and the periods of normal ECG recording.
Frank’s blood tests showed normal electrolyte levels and thyroid function.
Q5. What investigations are now indicated for Frank?
Frank should initially have a 24-hour Holter monitor, a cardiac echocardiogram and an exercise stress test.
A cardiac event monitor or an implantable cardiac loop recorder may be of value for further symptom–rhythm correlation if the patient does not have symptoms or electrical abnormalities that are diagnostic during the 24-hour Holter monitor. Event monitors and loop recorders can monitor the electrical activity of the heart continuously and record relevant snapshots, as did Frank’s smartphone app. They can transmit to the cardiologist when episodes are recorded. Episodes may be recorded automatically if the device detects high or low heart rates, a pause or atrial fibrillation. The patient can also press a button to store an episode if they have symptoms. Some apps on smartphones, watches and tablets can perform similar functions.
Implantable devices can remain in place for up to five years.
Q6. What are the common types of pacemaker and their indications?
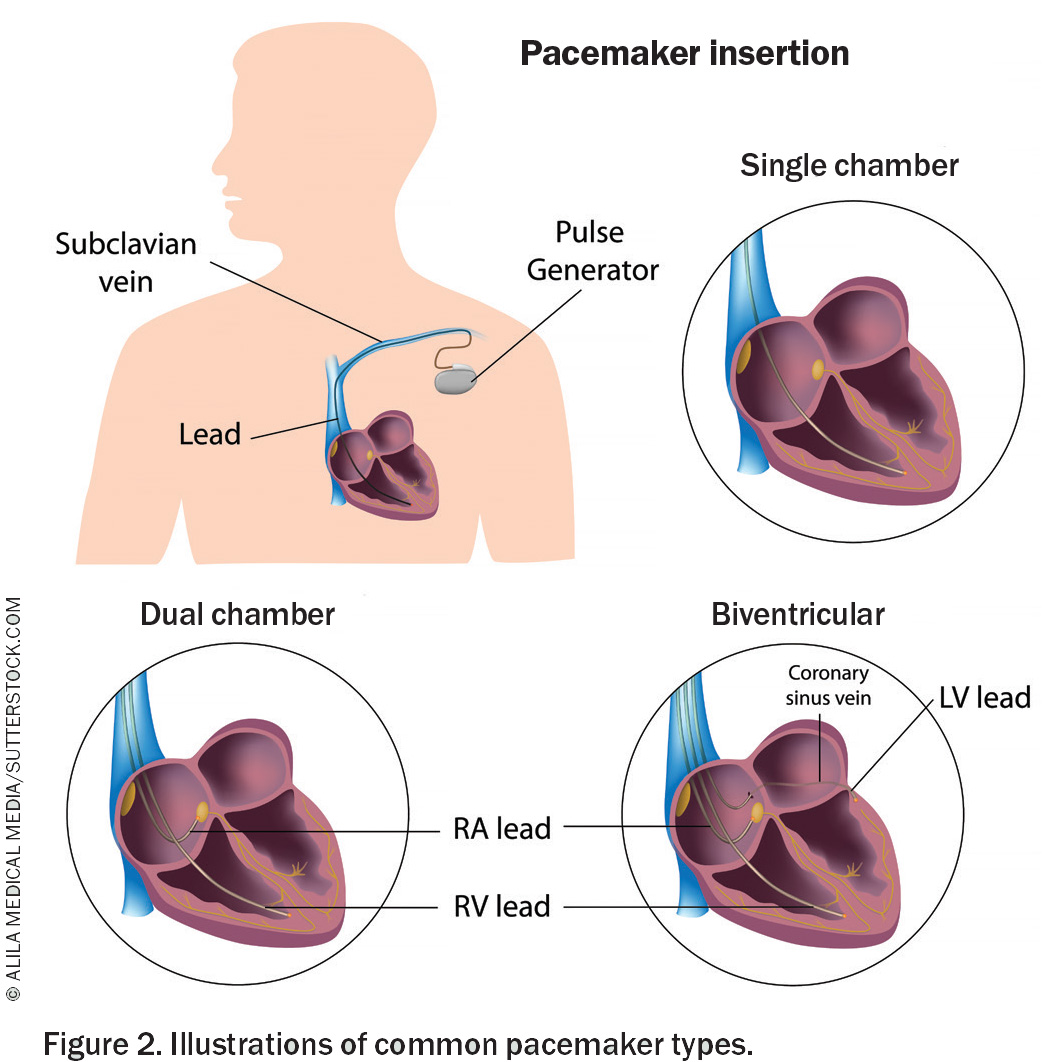
Common types of pacemaker are listed below, and shown in Figure 2.2
- Single-chamber pacemaker, which has a single lead going to either the upper (atrial) or lower (ventricular) cardiac chambers. There is also a leadless version, implanted in the right ventricle via a delivery system from the femoral vein; this is particularly useful in patients with poor subclavian venous access.
- Dual-chamber pacemaker, which has one lead going to the atrium and one to the ventricle.
- Biventricular pacemaker, which is used for cardiac resynchronisation therapy (see below).
Conduction system pacing is a relatively new technique in which a single ventricular pacing lead is implanted into the interventricular septum to capture the conduction system (His bundle or left bundle branch). This achieves more synchronised ventricular contraction than a traditional pacing lead implanted into the ventricular myocardium.
An implantable cardioverter defibrillator and pacemaker may be inserted if this is needed for patients at risk of ventricular tachycardia or fibrillation.
The most common indications for pacemakers are as follows:
- sinus node dysfunction
- acquired AV block (e.g. after a myocardial infarction)
- heart failure with left bundle branch block (resynchronisation pacing)
- congenital heart block.2
Q7. What is cardiac resynchronisation therapy and when is it indicated?
Cardiac resynchronisation stimulates atria and ventricles to synchronise better with each contraction and so is used in patients with heart failure. These patients are symptomatic and have a left ventricular ejection fraction of 35% or lower.2 They typically have left bundle branch block or other significant intraventricular block.
Cardiac resynchronisation is also indicated in patients who have chronic atrial fibrillation that has been difficult to control and who have New York Heart Failure classification III or IV. In these patients, if incomplete biventricular pacing is present, AV node ablation may be needed to prevent the unwanted conducted beats.
Q8. What are the basic types of pacing modes?3,4
The basic types of pacing modes are as follows.
- AAI (atrial pacing and sensing, and inhibition response to a sensed impulse) or ‘atrial demand mode’ is a pacemaker mode used in sinus node dysfunction.
- VVI (ventricular pacing and sensing, and inhibition response to a sensed impulse) pacemaker mode is used if the atria are chronically in fibrillation but AV conduction is poor or highly variable.
- DDD (demand pacing and sensing, and dual inhibiting/triggering response to sensed impulses) pacemaker mode detects both the atrial and ventricular electrical activity. It is the most common pacemaker mode used.
- Rate-responsive pacing (e.g. AAIR or VVIR or DDDR modes) refers to the pacemaker’s automatic adjustment of pacing rate faster or slower depending on the patient’s activity, as detected by the pacemaker (using sensors that detect the patient’s movement, breathing rate or both).
As noted above, conduction system pacing is a method in which a lead is placed in the basal interventricular septum to capture the ventricular conduction system.
Outcome
The GP discussed the case briefly with Frank’s cardiologist, who asked that Frank be referred to him promptly. The metoprolol was ceased. The cardiologist obtained a resting cardiac echocardiogram and stress echocardiogram, which were normal.
Frank had an implantable loop recorder inserted, which in the first month showed further episodes of sinus arrest of 3 to 5 seconds. Frank fainted when the arrest was 4.5 seconds in duration but did not injure himself. He was stopped from driving and elected to have a permanent pacemaker inserted. His knee replacement was delayed until he had recovered from the implantation.
Frank was permitted to resume driving two weeks after the pacemaker implant. He was permitted to undergo MRI scanning of his knee once his pacemaker had been in place and functioning adequately for six weeks. CT
COMPETING INTERESTS: None.
References
1. ECG & Echo Learning [Internet]. Clinical ECG interpretation. Section 2, Chapter 9. Sinoatrial arrest & sinoatrial pause (sinus pause/arrest). Available online at: https://ecgwaves.com/topic/sinoatrial-arrest-sinoatrial-pause-sinus/ (accessed September 2023).
2. Glikson M, Nielsen JC, Kronborg MD, et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J 2021; 42: 3427-3520.
3. Lak HM, Goyal A. Pacemaker types and selection. Stat Pearls [Internet]. Last update: December 15, 2022. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK556011/ (accessed September 2023).
4. Burns E, Buttner R. Pacemaker rhythms – normal patterns. Life in the Fast Lane [Internet]. 2022. Available online at: https://litfl.com/pacemaker-rhythms-normal-patterns/ (accessed September 2023).