‘My heart feels like it’s fluttering, Doctor’
Articles in this section are inspired by, but not based on, real cases to illustrate the importance of knowledge about ECGs in relation to clinical situations in general practice. Management is not discussed in detail.
- Ventricular ectopic beats result in an ECG with abnormal, broader QRS complex appearance; however, they are mostly benign.
- Factors associated with increased risk for ventricular ectopic beats include hypertension, left ventricular hypertrophy and ageing.
- Precipitating factors for ventricular ectopic beats can be psychological (e.g. emotional stress), physiological (e.g. exercise) and biological (e.g. thyrotoxicosis, severe iron deficiency anaemia).
- A resting cardiac echo, 24-hour Holter monitoring and consideration of referral to a cardiologist are keystones of investigation and management.
- Patients with uncomplicated ventricular ectopic beats occurring in less than 15% of a 24-hour period most often do not require antiarrhythmic drug treatment.
Farah is a 90-year-old English-speaking Persian woman well known to your general practice. She frequently attends for a wide variety of possible symptoms and signs of illness. She becomes anxious about her health (which may explain why she has remained so well over the years). Her medical history includes long standing inactive Hashimoto’s disease, osteoporosis, cataract surgery and diverticulosis.
She is quite mobile and slim, has never smoked and does not drink alcohol. She lives with her daughter, son-in-law and grandchildren. Her medications include 100 mcg thyroxine daily and denosumab every six months. Her thyroid function test results have been stable for years, the last test being a month ago. On this same blood test, she had mild renal impairment (estimated glomerular filtration rate 50 mL/min/1.73 m2), a normal full blood count, electrolytes, serum calcium and magnesium levels and liver function. She has never needed cholesterol-lowering treatment and is normoglycaemic. Farah’s blood pressure ranges between 105/65 mm Hg and 135/85 mm Hg.
Farah makes an urgent appointment on a Monday morning after noticing her heart ‘fluttering’ over the weekend. She felt this during waking hours, including when she is dozing in the early morning. It was not constant but lasted hours and also disappeared for hours. She has not had this sensation before and has not attempted to count the speed or note any other features of her heart rate. She has not had syncope, presyncope or falls.
She has no past cardiac history, although she was assessed for atypical chest pain when she was 82 years of age. At that time, the CT angiogram showed minimal generalised atheroma, the coronary artery calcium score was 96 and the resting cardiac echo was normal apart from mild mitral valve regurgitation.
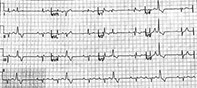
An ECG is performed as part of a cardiac investigation (Figure).
Q1. What does this ECG show?
The ECG shows trifascicular block with sinus rhythm 75 beats/min (corrected QT 421 to 473 ms), frequent premature ventricular ectopic beats, first-degree atrioventricular (AV) block, marked left axis deviation, left anterior fascicular block (broad R or R’ in V1 or V2, QRS axis superior to −30 degrees) and right bundle branch block. These are indicative of diffuse conduction system disease in addition to ventricular ectopy.
Q2. What are ventricular ectopic beats?
Ventricular ectopic beats are premature beats arising from an ectopic focus within the ventricles. They are also known as premature ventricular beats, premature ventricular complexes and ventricular extra systoles.1
Depolarisation from electrical activity in the heart normally begins in the sinoatrial node (where the impulse is fastest) and travels down to the atrioventricular nodes (where the impulse is slowed) and through the His-Purkinje system throughout the ventricular muscle. Pacemaker cells within the ventricular system may spontaneously depolarise; however, this electrical activity is usually suppressed by the faster electrical impulses coming from above this level.
A resting cardiac echo should be arranged as ventricular ectopic beats occur when an ectopic focus in the ventricle produces an electrical impulse that is independent of the His-Purkinje system and is, therefore, not connected with it. This causes a contraction of the ventricles, with a different activation pattern to a conducted sinus beat. The result is an abnormal-appearing, broader QRS complex on the ECG (over 120 ms in duration). There are also ST and T wave changes and commonly a compensatory pause afterwards.1 If the ectopic beat occurs in the atrium, it is an atrial ectopic beat; if it occurs in the atrioventricular junction, it is a junctional ectopic beat.
Ventricular ectopic beats may be monomorphic or polymorphic. If they are monomorphic, each beat appears the same on the ECG trace because they arise from the same ectopic focus. Beats arising from multiple ectopic foci within the ventricle appear different to each other and are called polymorphic.
Q3. Are ventricular ectopic beats dangerous?
Ventricular ectopic beats may be associated with runs of ventricular tachycardia. It is quite common for the ventricular ectopic beats to originate from the right ventricular outflow tract.2 These beats are distinct in that the QRS complexes have a left bundle branch block with an inferior axis morphology. This is one of the common sites of origin of ectopic beats or ventricular tachycardia in patients with normal hearts. These patients are more often aged between 20 and 40 years and are more likely to be female.2
Vagal stimulation may suppress ventricular ectopic beats and hence reduced vagal stimulation after exercise is associated with these beats. An increased risk of cardiovascular death over 5.3 years of follow-up was seen in patients with no history of heart failure, arrhythmias or valvular disease, but who had increased ventricular ectopic beats (more than seven per minute, or bigeminy or trigeminy, ventricular tachycardia or ventricular fibrillation) in the recovery phase of a stress test.3 By and large; however, ventricular ectopic beats are benign.
The ARIC (Atherosclerosis Risk in Communities) Study showed that increased left ventricular mass was associated with increased ventricular ectopic beats. Hence hypertension, left ventricular hypertrophy and ageing were factors also associated with an increased risk of ventricular ectopic beats.4 It is unknown whether the slightly increased incidence of sudden cardiac death associated with very frequent ventricular ectopic beats is due to the underlying pathological process or the ectopic beats themselves causing fatal arrhythmias.5
Q4. What is the differential diagnosis of Farah’s symptoms?
Farah is most likely having short runs of ventricular tachycardia or is simply sensing some of the isolated ectopic beats as palpitations. Other possibilities to consider include:
- atrial fibrillation
- frequent atrial or ventricular ectopic beats
- short and repeated runs of supraventricular tachycardia
- second-degree AV block.
Q5. Does Farah need further investigations or management?
The combination of first-degree AV block and bifascicular block (right bundle branch block and left anterior fascicular block) suggests possible trifascicular conduction disease, with increased risk of high-grade AV block, and for these reasons, atrial fibrillation must also be considered. Farah needs a 24-hour Holter monitoring study. She has underlying conduction system disease (trifascicular block), so Holter monitoring will also be important to exclude asymptomatic episodes of higher-grade AV block.
Ventricular ectopic beats can be associated with left ventricular dysfunction. A referral to a cardiologist should be discussed with Farah, with a view to possible medical management of the frequent ectopic beats, especially if echocardiography shows a reduced ejection fraction or dilation of the ventricles (as this may be associated with more than approximately 15% ventricular ectopic beats in a 24-hour period). It is not necessary to repeat the thyroid function tests but the full blood count, electrolytes, kidney function and iron studies should be reviewed.
Q6. What can you tell Farah about why this problem has suddenly started, assuming her test results are normal.
Frequent ventricular ectopic beats may be precipitated by exercise, emotional stress, thyrotoxicosis (which Farah does not have), sympathomimetic medications, alcohol, severe iron deficiency anaemia and other causes of cardiac ischaemia, hypomagnesaemia and hypokalaemia, and age-related changes in the cardiac electrical conduction system (which Farah has evidence of on her ECG).
A high caffeine intake (9 or more cups a day) may precipitate ventricular ectopic beats in people with a susceptibility towards cardiac conduction defects, but average caffeine intake does not appear to be significantly correlated with ventricular ectopic beats.2 Caffeine restriction does not appear to significantly decrease ventricular ectopic beats.2
Q7. Should Farah be treated for frequent ventricular ectopic beats and, if so, what issues should be considered?
The main reason for treating Farah is if there is a risk that the frequency of the ventricular ectopic beats could adversely affect her left ventricular function. In contemporary practice, a threshold of above 15% of all heart beats is regarded as sufficient to lead to a reversible cardiomyopathy. Holter monitoring and a resting cardiac echo will aid management decisions. If the results of these are unremarkable then there is probably no need to offer any therapy beyond reassurance (which in itself is often helpful).
Medications that could be considered to reduce ventricular ectopic beats include sotalol, amiodarone (contraindicated in this case as Farah has hypothyroidism) and flecainide (which may be paradoxically proarrhythmic and associated with increased risk of death in patients with coronary or structural heart disease).2 Serious side effects of treatment include hypotension, bradycardia and the possibility of precipitating heart block. These complications may also significantly increase the risk of falls. If Holter monitoring discloses higher grade AV block, a pacemaker may be needed. However, in Farah’s case, it is hard to justify any antiarrhythmic drug therapy, and if her symptoms worsen or continue to trouble her, referral to a cardiologist should be the next step.
Loop recorder implantation can be a useful way of investigating and monitoring patients with palpitations and risk of AV block. Catheter ablation can be performed for medically refractory ventricular ectopic beats.
Outcome
Farah continues to have frequent ventricular ectopic beats for many hours daily (12% of a 24-hour period), confirmed on 24-hour Holter monitoring, with no high- grade AV block and no atrial fibrillation. She has normal blood test results and an ECG shows stable mild mitral regurgitation and mild HFPEF (heart failure with preserved ejection fraction, previously known as diastolic dysfunction). A cardiologist’s opinion is obtained and it is decided after discussion with Farah not to treat the ventricular ectopic beats. Farah finds after a few more weeks that she does not notice them as often and this reassures her greatly. CT
References