FitBit and an irregular pulse
Articles in this section are inspired by, but not based on, real cases to illustrate the importance of knowledge about ECGs in relation to clinical situations in general practice. Management is not discussed in detail.
- In atrial fibrillation, the atria contract irregularly and continuously; on the ECG the RR interval is variable, discrete P waves are absent and the baseline undulates. The ventricular response is variable and may be slow, normal or fast.
- Second-degree atrioventricular (AV) block is where all beats are conducted but with a longer-than-normal PR interval due to conduction problems through the AV node between the atria and the ventricles.
- Mobitz type 1 second-degree block (Wenckebach) is where there is progressive shortening of the RR duration with each beat until one beat is not conducted. The PR interval is constant.
- Mobitz type 2 second-degree heart block is where the PR interval remains constant but there are dropped beats with preservation of the P waves alone, present in multiples of the number of preceding beats. Therefore the RR interval around the dropped beats is an exact multiple of the preceding RR interval.
- Third-degree (‘complete’) heart block is where there is no conduction to the ventricles so any ventricular rhythm is an ‘escape’ rhythm, usually from the His-Purkinje conduction system.
- Generally, patients with second-degree AV block in sinus rhythm have slower ventricular rates if their atria are in fibrillation than patients with normal AV conduction (in the absence of AV node-blocking medications).
- Medications that slow the electrical conduction through the AV node (beta blockers, nondihydropyridine calcium channels antagonists such as diltiazem and verapamil, and digitalis) may cause high-grade heart block.
- A 10-second ECG rhythm strip may be crucial for diagnosis and the ECG is incomplete without it.
Saira, a 77-year-old woman, has just moved to your practice as her previous GP retired. She is organised and motivated and on her first visit presented you with all her medical history. On this, her second visit, you are preparing a chronic disease management plan for her physiotherapy and podiatry appointments. She has a 10-year history of type 2 diabetes (her latest HbA1c level was 6.9% a month ago; she is taking metformin 1 g twice daily and sitagliptin 10 mg daily) and hypertension (fairly well controlled on diltiazem CD 180 mg in the morning and candesartan 16 mg at night). She tells you she suffers from anxiety, and the diltiazem tends to reduce her pulse rate too. She also takes atorvastatin 40 mg in the morning, fluticasone 250 mcg/salmeterol 25 mcg inhaler, two inhalations twice daily, and thyroxine 75 mg in the morning. Her last routine blood tests, including iron studies and thyroid function tests, were performed a month ago and were normal.
Saira last saw a cardiologist two years ago for atypical chest pain and at that time her coronary artery CT angiogram showed diffuse atherosclerosis with maximum 35% blockages. She did not require an angiogram at the time and has been medically managed since then.
At the end of the consultation, just as you hand Saira her paperwork, she tells you that her retirement village had organised an exercise physiologist to review all residents and she had been persuaded to spend $139 on a FitBit. She says that since she has started wearing this, her pulse has been irregular, ranging from 40 beats/minute to 110 beats/minute, and the FitBit has alerted her to frequent alarms. Saira has ignored these as she was coming to see you anyway and she feels well, even during the mild exercise she has been undertaking.
Your heart sinks as you feel her pulse. It is irregularly irregular and the rate is approximately 85 beats/min. Her blood pressure is 147/95 mmHg. Saira says she has felt perfectly normal apart from her concern about her pulse. You organise an ECG, but the paper runs out before you can print a rhythm strip.
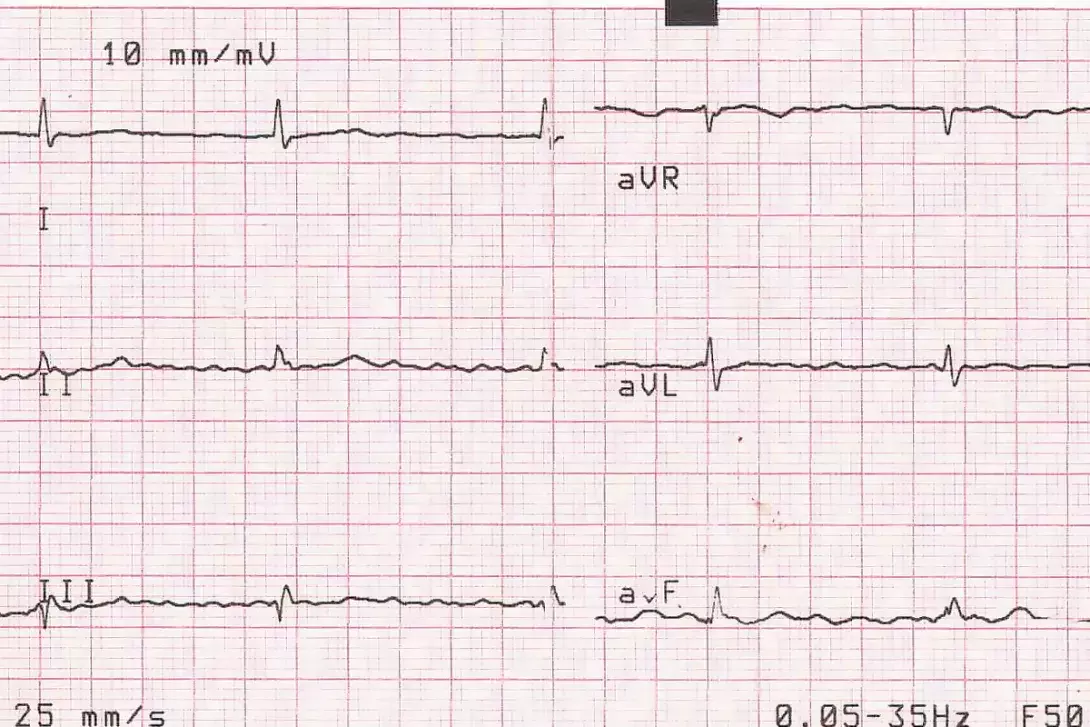
Q1. What does the ECG show?
The ECG shows either atrial fibrillation (AF) (‘coarse’) or atrial flutter with a slow irregular ventricular conduction. There appears to be a rapid atrial rate of over 300 ms. The heart rate is 68 beats/minute and the QTc is 422 ms.
The absence of a rhythm strip makes the true diagnosis more difficult to make. It is also possible that this is a high-grade (second- or third-degree) heart block with rapid AF (at a rate of 300 ms).
Q2. What is atrial fibrillation and what could it be caused by in this patient?
In AF, the atria contract irregularly and continuously and so the RR interval is variable, discrete P waves are absent and the baseline undulates. The ventricular response is variable and may be slow (‘slow AF’), normal or fast (‘rapid AF’). The pulse rate recorded by blood pressure measurement, FitBit or SmartWatch is often slower than the actual ventricular rate seen on an ECG recording. This is because some beats (the ones that happen soon after the previous beat) produce no detectable pulse because the heart has had little time to fill with blood after the preceding beat.
AF is the most common type of tachyarrhythmia. Causes to be considered in this patient include:
- age
- ischaemic heart disease
- valvular disease
- cardiomyopathy
- hypertensive heart disease
- hyperthyroidism (the patient has normal thyroid function)
- myocarditis (unlikely and asymptomatic)
- pulmonary emboli (unlikely in the absence of precipitants, symptoms and no previous history of venous thromboembolism)
- drug and alcohol intoxication
- severe metabolic derangements (especially relating to electrolytes and anaemia, neither of which the patient has).
Salbutamol and salmeterol are beta agonists that have been associated with AF, but this is uncommon without other causes unless used in excess. The condition may occur spontaneously in the absence of heart disease or precipitants.
Q3. What is second-degree heart block?
Second-degree atrioventricular (AV) block is the intermediate grade of heart block, between first-degree (where, in sinus rhythm, all beats are conducted but with a longer-than-normal PR interval) and third-degree (‘complete’) heart block.
In second-degree AV block, all beats are conducted but with a longer-than-normal PR interval) due to conduction problems through the AV node between the atria and the ventricles. Mobitz type 1 second-degree block (Wenckebach) is where there is progressive shortening of the RR duration with each beat until one beat is not conducted. The PR interval is constant. Mobitz type 2 second-degree heart block is where the PR interval remains constant, but there are dropped beats with preservation of the P waves alone, which are present in multiples of the number of preceding beats. Therefore, the RR interval around the dropped beats is an exact multiple of the preceding RR interval.
In third-degree heart block there is no conduction to the ventricles so any ventricular rhythm is an ‘escape’ rhythm, usually from the His-Purkinje conduction system. The distance from R to R is quite regular in third-degree AV block. The QRS complex is wide if the origin of the escape rhythm is in the distal conduction system or ventricular myocardium.
In this case, the QRS complex is normal and the ventricular rhythm is irregular, consistent with conduction occurring through the AV node. In sinus rhythm, second-degree AV block is defined by some sinus beats being conducted and some not (in Mobitz type 1 or 2 or 2:1 pattern). Generally, patients with second-degree AV block in sinus rhythm have slower ventricular rates if their atria are in fibrillation than patients with normal AV conduction (in the absence of AV node-blocking medications).
Q4. What are the possible causes of second-degree heart block in this patient?
The medical causes of high-grade (second- or third-degree) heart block are, most often, myocardial ischaemia, fibrosis, calcification and cardiomyopathy. Transient high-grade heart block is often caused by inferior wall myocardial ischaemia, which may affect the AV node.
Medications that slow the electrical conduction through the AV node, including diltiazem, which Saira is taking, may cause high-grade heart block. Other such medications include beta blockers, other nondihydropyridine calcium channels antagonists (e.g. verapamil) and digitalis.
Idiopathic conduction defects, trauma, lupus and infiltration disorders (such as amyloidosis and haemochromatosis (this patient has normal iron studies) can cause high-grade heart block.
Complete heart block may occur in patients who have myocarditis, or with an underlying cardiomyopathy.
Q5. What is the recurrence risk of high-grade heart block (if this was present in this case) after ceasing diltiazem?
To determine the recurrence risk of AV block after ceasing AV-blocking medications, one research group compared two groups of patients with second- or third-degree AV block that was not caused by myocardial ischaemia, digitalis toxicity or vasovagal issues.1 In one group, 77 patients were not taking medications known to cause an AV block and in the other, 92 patients were initially on such medications (beta blockers and/or diltiazem or verapamil).
The study found that ceasing the medication that caused AV block almost doubled the chance of the AV block resolving (41%) compared with spontaneous resolution in patients who were not taking such medications (23%). However, a significant number of patients whose medication had been ceased still had an AV block (59%). In addition, 56% of patients who had complete resolution of the AV block after ceasing medication had a recurrence of the AV block within three weeks. It was concluded that only 15% of all patients who had an AV block had a true ‘cure’ over the study period after ceasing the medication that was associated with this condition.
Outcome
The absence of a 10-second rhythm strip may lead to misdiagnosis of certain arrhythmias. Without this rhythm strip, each lead will only span 2.5 seconds. Lead II in particular can offer diagnostic information, especially pertaining to P waves, that may not be clear in the other leads. In Saira’s case, the arrhythmia was transient and by the time a second ECG with a rhythm strip was organised she was in sinus rhythm. A Holter monitor was arranged and this showed Wenckebach phenomenon. This offers more diagnostic evidence that the original ECG was most likely a second-degree heart block (rather than, for example, a third-degree block) slowing down the concurrent rapid AF.
The cardiologist was contacted and Saira was prescribed apixaban 5 mg twice daily for prevention of stroke and other thromboembolism. She was given appropriate warnings regarding potential bleeding risks. The diltiazem CD had been achieving appropriate rate control, so this medication was continued. If tachycardia was a problem, the salmeterol component of the combination inhaler could be reduced or stopped, with vigilance for worsening of asthma control. A cardiac echocardiogram was performed and this was essentially normal.
Rhythm control has been found to have prognostic benefit (reduced risk of composite outcome of death from cardiovascular causes, stroke, or hospitalisation with worsening of heart failure or acute coronary syndrome) even in asymptomatic patients.2
Rhythm control may be achieved by a combination of cardioversion(s), antiarrhythmic medication and catheter ablation, tailored according to the patient’s individual comorbidities, symptoms and responses to treatments.
Many patients have a degree of sinus-node dysfunction as well as AF. The combination is known as tachy-brady syndrome and a permanent pacemaker implant may be indicated if the bradycardia component is symptomatic or is limiting medication treatment of the fibrillation.
COMPETING INTERESTS: None
References
1. Zeltser D, Justo D, Halkin A, et al. Drug-induced atrioventricular block: prognosis after discontinuation of the culprit drug. J Am Coll Cardiology 2004; 44: 105-108.
2. Kirchhof P, Camm AJ, Goette A, et al, for the EAST-AFNET 4 Trial Investigators. Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med 2020; 383: 1305-1316.
