INOCA: frequently misdiagnosed and poorly treated

Ischaemia with nonobstructive coronary arteries (INOCA) is under-recognised and undertreated. Treatment is tailored to the patient, and dependent on the identified subtype and its underlying aetiology.
- Ischaemia with nonobstructive coronary arteries (INOCA) is an increasingly recognised cause of angina in the absence of 50% or more obstructive coronary artery disease.
- There are three different subtypes of INOCA: INOCA due to microvascular dysfunction, INOCA due to epicardial vasospasm and INOCA due to a combination of both microvascular dysfunction and vasospasm.
- INOCA can be diagnosed invasively or noninvasively, but the gold standard is invasive functional coronary angiography. This procedure can also exclude obstructive ischaemia as a cause of chest pain.
- Medical therapy for patients with INOCA needs to be personalised, guided by the subtype of INOCA that a patient experiences, and includes the use of cardioprotective medications and symptomatic treatments.
Ischaemia with nonobstructive coronary arteries (INOCA) is defined as the presence of myocardial ischaemia in the absence of coronary artery disease with more than 50% obstruction. Patients with INOCA are known to have impaired quality of life, increased use of healthcare resources utilisation, and a disconcerting risk of major cardiovascular events compared with the general population; despite this, patients remain suboptimally managed. This article provides an overview of INOCA and highlights the key management principles that all GPs should be aware of in managing patients with INOCA in daily practice.
INOCA has become an increasingly recognised cause of angina, particularly over the past decade. It is described as having evidence of myocardial ischaemia, whether obtained by stress electrocardiography, cardiac stress imaging or functional coronary angiography, that occurs in the absence of obstructive coronary artery disease. INOCA can be difficult to diagnose and remains under-recognised and undertreated. Significant efforts have been made recently by world-leading experts to encourage appropriate recognition and management of this condition, which is associated with increased morbidity and mortality compared with the general population.1
Subtypes
INOCA results from a mismatch of coronary perfusion and myocardial oxygen demand because of impaired coronary blood flow. This may arise from coronary microvascular dysfunction, epicardial artery spasm or a combination of both; these are the three subtypes of INOCA (Box).2
Risk factors
Traditional cardiovascular risk factors (e.g. older age, smoking, hypertension and diabetes mellitus) have been associated with INOCA, as well as chronic autoimmune conditions. Although there is a similar prevalence of INOCA in men and women, there are several sex-specific risk factors identified for women, including gestational diabetes, pre- eclampsia/eclampsia and menopause. Migraines and Raynaud’s phenomenon also commonly occur in patients with coronary artery spasm, as they are prone to vasoconstriction in multiple vascular beds.4
Adverse outcomes
It is known that INOCA itself is not benign. Patients with angiography-confirmed obstructive coronary artery disease have a high risk of major cardiovascular events (MACE) compared with those who have INOCA. However, mounting evidence suggests that patients with INOCA have a higher risk of MACE compared with the general population.5 This patient population is also recognised to have an impaired quality of life and be more likely to use healthcare resources recurrently.3,6 This is partly related to an under-recognition of the condition by clinicians, but also to the fact that there are limited treatment options.
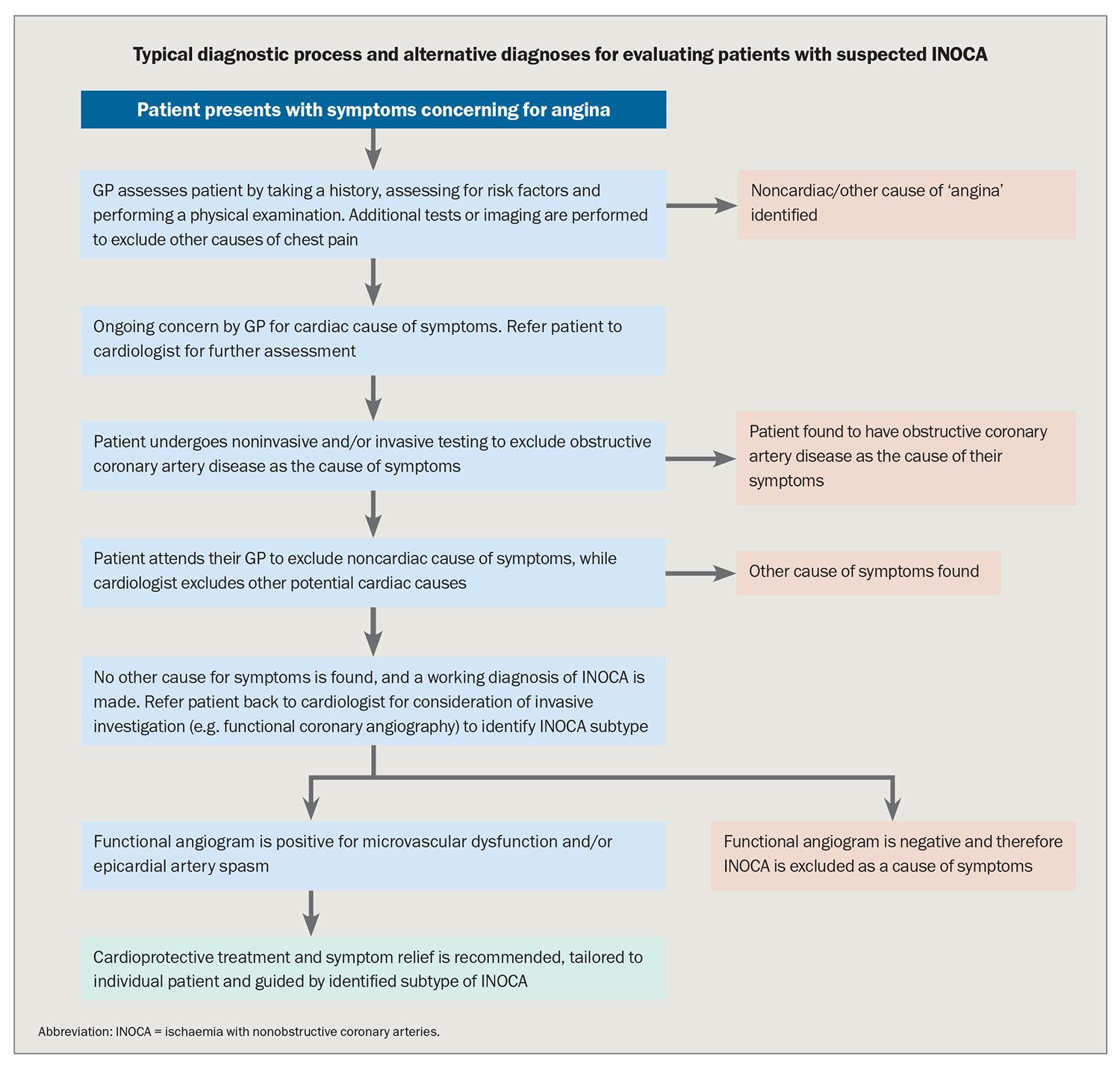
Clinical suspicion and diagnosis
It is often assumed that angina is caused by flow-limiting atherosclerotic coronary stenoses, but this is not always the case.1 Up to half of patients who present for elective invasive coronary angiography for the investigation of stable chest pain or angina will continue to experience symptoms despite an apparently ‘normal’ test result.2 Many of these patients will be labelled as having ‘noncardiac chest pain’ and told that nothing is wrong, while they continue to experience symptoms.
The GP has a key role in the assessment of these patients, as they are often discharged back to their care following ‘normal’ angiography. Other noncardiac causes, such as gastro-oesophageal reflux disease, oesophageal dysmotility and gallstones, should be excluded, with specialty referrals as appropriate.
Although INOCA is a chronic condition, patients can still present with acute, prolonged chest pain. If there is any doubt regarding the aetiology of the pain, referral to a local emergency department for acute investigations (such as serial troponins and ECG) should be considered.
Investigation of INOCA
INOCA is a ‘working diagnosis’ that requires identification of the underlying cause so treatment can be appropriately targeted. This is best achieved with prompt referral to a cardiologist, with details outlined in the Flowchart.
Functional coronary angiography
Functional coronary angiography is a specialised form of invasive coronary imaging that evaluates the presence of coronary macrovascular and microvascular dysfunction. In contrast, conventional invasive coronary angiography and coronary CT angiography evaluate the coronary circulation as ‘large rigid pipes’ (i.e. structural coronary angiography), and do not routinely assess the dynamic nature of the large epicardial coronary arteries (i.e. epicardial artery spasm), nor the coronary microcirculation. Indeed structural coronary angiography assesses only 5% of the coronary circulation.
In functional coronary angiography, the following assessments are undertaken:
- exclusion of any suspicious obstructive atherosclerotic coronary lesions by measuring the lesion pressure gradient via fractional flow reserve measurements
- evaluation of coronary microvascular dysfunction by measuring coronary blood flow/resistance in response to adenosine (a potent coronary microvascular vasodilator)
- coronary spasm provocation testing with acetylcholine.
The procedure is undertaken during standard diagnostic invasive coronary angiography but does require specialised equipment and training. At the completion of functional coronary angiography, the subtypes of INOCA can be distinguished and more specific targeted therapy considered.
Noninvasive procedures
Cardiac positron emission tomography, cardiac MRI and stress contrast echocardiography are all noninvasive techniques to assess myocardial blood flow/perfusion and thus evaluate the presence of coronary microvascular dysfunction. However, these highly specialised coronary blood flow imaging modalities are seldom used for the routine clinical diagnosis of coronary microvascular dysfunction in Australian hospitals.
Treatment
The care of patients with INOCA should be closely co-ordinated between the GP and cardiologist because of the difficulty with determining the diagnosis, the potential psychosocial impact of the diagnosis, and the recognition that symptoms often fluctuate. A thorough assessment, using invasive functional coronary angiography, followed by targeted medical therapy for identified INOCA subtypes, improves outcomes for patients.7,8 Hence, a personalised approach to treating these patients is important, treating these patients is important, in changing prognosis, ameliorating symptoms and improving overall health status, thereby, improving quality of life.9
Defining the mechanism driving INOCA is important because treatments vary between the subtypes; for example, beta blockers are useful in the treatment of microvascular dysfunction but likely to exacerbate epicardial artery spasm. Patient responses to treatments can differ, which further highlights the importance of personalised treatment. Cardioprotective treatments including statins, ACE inhibitors, diabetic therapies and appropriate weight loss measures, are often recommended for patients with INOCA. Trials are in progress to evaluate whether cardioprotective medications are efficacious in improving outcomes in patients with INOCA.10
Treatments such as calcium channel blockers, nitrates or nicorandil are likely to provide the greatest symptomatic relief for patients with epicardial artery spasm, although it is recognised that individuals will have varying responses and usually multiple agents are required to provide symptomatic relief. For microvascular dysfunction, beta blockers are the preferred antianginal agent.
Smoking cessation for all active smokers should be strongly encouraged, and stress coping strategies may be required, as stress can often precipitate angina, or worsen it in patients with refractory symptoms. Patients should also be educated to avoid any precipitating factors; this is particularly important in those with epicardial artery spasm, in whom several recreational drugs (including alcohol, cocaine, cannabis, amphetamines and several antimigraine medications) have been recognised to trigger symptoms. Cardiac rehabilitation is well established and recommended in clinical guidelines for obstructive atherosclerotic coronary artery disease, with its use in people with INOCA being investigated.
There is ongoing interest in the development of novel agents for the treatment of INOCA, particularly those targeting the inflammatory pathway. Given the suboptimal management of most patients with INOCA, having access to cutting edge clinical trials is important. Patients should be encouraged to keep in touch with their regular cardiologist in case of changes in management recommendations.
Useful information resources
Patients with INOCA can experience distress, with many having fluctuating symptoms and some having refractory symptoms, despite taking several antianginal medications. Support is usually required to help patients learn to live with their condition, in addition to information received from health care professionals.
Patient support groups including INOCA International (https://www.inocainternational.com/) and the International Heart Spasms Alliance (https://www.internationalheartspasmsalliance.org/), are available to help patients interact with others who have similar issues. The Coronary Vasomotor Dysfunction International Study (COVADIS) group has developed seminal papers for clinicians detailing the diagnostic criteria for coronary vasomotor disorders (https://covadis.online/).
Conclusion
Despite the significant cardiovascular risk to patients, INOCA remains under-diagnosed and poorly managed. GPs are positioned well to recognise INOCA and should consider the diagnosis in patients with a history highly suggestive of angina and in whom other causes have been ruled out and obstructive structural coronary artery disease has been excluded. Further assessment of patients with referral to a cardiologist is essential. Determining the aetiological subtype of INOCA provides guidance on treatment, which should be holistic and tailored to the individual patient, and aim to relieve symptoms and improve prognosis, overall health status and quality of life. CT
COMPETING INTERESTS: None.
References
1. Boden WE, Marzilli M, Crea F, et al. Evolving management paradigm for stable ischemic heart disease patients: JACC Review Topic of the Week. J Am Coll Cardiol 2023; 81: 505-514.
2. Kunadian V, Chieffo A, Camici PG, et al. An EAPCI expert consensus document on ischaemia with nonobstructive coronary arteries in collaboration with European
Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation endorsed by Coronary Vasomotor Disorders International Study Group. Eur Heart J 2020; 41: 3504-3520.
3. Tavella R, Cutri N, Tucker G, Adams R, Spertus J, Beltrame JF. Natural history of patients with insignificant coronary artery disease. Eur Heart J Qual Care Clin Outcomes 2016; 2: 117-124. 4. Beltrame J, Crea F, Kaski J, et al. The who, what, when, how and where of vasospastic angina. Circ J 2016; 80: 289-298.
5. Jespersen L, Abildstrom SZ, Hvelplund A, et al. Burden of hospital admission and repeat angiography in angina pectoris patients with and without coronary artery disease: a registry-based cohort study. PLoS One 2014; 9: e93170.
6. Radico F, Zimarino M, Fulgenzi F, et al. Determinants of long-term clinical outcomes in patients with angina but without obstructive coronary artery disease: a systematic review and meta-analysis. Eur Heart J 2018; 39: 2135-2146.
7. Ford TJ, Stanley B, Good R, et al. Stratified medical therapy using invasive coronary function testing in angina: the CorMicA trial. J Am Coll Cardiol 2018; 72: 2841-2855.
8. Ford TJ, Stanley B, Sidik N, et al. 1-Year outcomes of angina management guided by invasive coronary function testing (CorMicA). JACC Cardiovasc Interv 2020; 13: 33-45.
9. Beltrame JF, Tavella R, Jones D, Zeitz C. Management of ischaemia with nonobstructive coronary arteries (INOCA). BMJ 2021; 375: e060602.
10. Handberg EM, Merz CNB, Cooper-Dehoff RM, et al. Rationale and design of the Women’s Ischemia Trial to Reduce Events in Nonobstructive CAD (WARRIOR) trial. Am Heart J 2021; 237: 90-103.