A woman with breathlessness: what is the underlying diagnosis?
Articles in this section are inspired by, but not based on, real cases to illustrate the importance of knowledge about ECGs in relation to clinical situations in general practice. Management is not discussed in detail.
- The cardiac ventricles are normally activated from the atria via the atrioventricular node and His-Purkinje system; ventricular ectopic beats occur when one or more ectopic foci in the ventricle produce an electrical impulse, causing a contraction that is not synchronised with the atrial contraction.
- Monomorphic ventricular ectopic beats may be associated with runs of ventricular tachycardia.
- Studies suggest that a rate of up to 100 ventricular ectopic beats in a 24-hour period on Holter monitoring is within normal limits.
- More than 5000 ventricular ectopic beats in 24 hours on Holter monitoring can be responsible for such frequent and irregular contraction of the myocardium that left ventricular dysfunction or dilated cardiomyopathy may develop.
- Ventricular ectopics that are not likely to be pathological tend to be abolished with significant exercise and return in the phase immediately after exercise.
Shayla, aged 48 years, has been a patient of your practice for many years. She presents for a telephone consultation with continuing shortness of breath on exertion since an illness six weeks ago.
Shayla takes candesartan 8mg daily as she was diagnosed with hypertension 10 years ago. She also takes atorvastatin 40mg daily and aspirin 100mg daily. She has no other medical problems and had normal blood test results six months ago. She believes she had coronavirus disease 2019 (COVID-19) a year ago and received the second dose of Comirnaty (Pfizer) two months ago.
Six weeks ago, Shayla developed a temperature of 38.0 to 38.5°C that lasted for five days. She had a headache, myalgia, a sore throat and a dry cough that became productive on day five. Notably, she had significant shortness of breath on any exertion, although it was not present at rest. She had no chest discomfort.
A PCR test for COVID-19 on day 2 of the illness had negative results. She consulted you by telephone, and you arranged serum antibody testing on day 4. This was negative for IgM but positive for IgG to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
A few days before her illness began, Shayla’s father died. He had been ill for over a month, and she had been travelling four hours daily several days a week to see him and her family, while continuing to work as much as possible. She felt this extreme pressure was partly why she was so unwell. Normally she is highly active, but she did not have time to exercise.
Shayla’s illness lasted five days, but the productive cough and shortness of breath continued. A chest x-ray a week after the illness began was reported as normal. The productive cough responded to doxycycline 100mg twice daily for seven days. However, the shortness of breath continued.
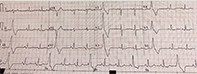
You refer Shayla to a respiratory specialist who fortuitously can see her immediately. Her lung function tests are normal, and asthma is excluded. The specialist notes an irregularly irregular pulse, rate 80 to 90 beats per minute, blood pressure of 138/90mmHg, a normal apex beat and no raised jugulovenous pressure or peripheral oedema. An ECG is arranged urgently (Figure).
Q1. What does this ECG show?
The ECG shows monomorphic ventricular ectopic beats in trigeminy. The heart rate is 84 beats per minute, and the corrected QT interval is 389 ms.
Q2. What are ventricular ectopic beats and what is their significance?
Ventricular ectopic beats are premature beats arising from an ectopic focus within the ventricles. They are also known as premature ventricular beats, premature ventricular complexes and ventricular extrasystoles.
Depolarisation from electrical activity in the heart normally commences in the sinoatrial node (where the impulse is fastest) and travels down to the atrioventricular nodes (where the impulse is slowed) and through the His-Purkinje system throughout the ventricular muscle. Pacemaker cells within the His-Purkinje system may spontaneously depolarise; however, this electrical activity is usually suppressed by the faster electrical impulses coming from above this level.
Ventricular ectopic beats occur when an ectopic focus in the ventricle produces an electrical impulse that is independent of the His-Purkinje system. This causes a contraction in the ventricles. The result is abnormal-appearing, broader QRS complexes (over 120ms duration) on the ECG. ST and T wave changes also occur, and often a compensatory pause afterwards.1 If an ectopic beat occurs in the atrium, it is an atrial ectopic; if it occurs in the atrioventricular junction, it is a junctional ectopic beat.
Ventricular ectopic beats may be monomorphic or polymorphic. If they are monomorphic, each beat appears the same on the ECG trace because they arise from the same ectopic focus. Beats that arise from multiple ectopic foci within the ventricle appear different to each other and are termed polymorphic. Monomorphic ventricular ectopic beats may be associated with runs of ventricular tachycardia.2
Ventricular ectopic beats are more likely in the context of alcohol consumption, high caffeine intake, use of medications (e.g. amphetamines, cocaine, tricyclic medications), a heightened adrenergic state, electrolyte abnormalities (low potassium, magnesium or calcium), hypoxia, hypercapnia, acute myocardial ischaemia, cardiomyopathies, myocarditis and mitral valve prolapse.3
Q3. What should be done next?
Shayla should have 24-hour Holter monitoring. She should also be advised to moderate her intake of caffeine and alcohol and to take a magnesium supplement daily. In view of the possibility of viral myocarditis and the frequent ectopic beats, blood tests to measure C-reactive protein, thyroid stimulating hormone and serum electrolyte levels, iron studies and a full blood count (to exclude anaemia) would also be reasonable. Measurement of serum troponin level could be considered, but this is unlikely to be abnormal now as the possible myocarditis occurred six weeks previously.
Shayla undergoes 24-hour Holter monitoring, which shows 22,630 ectopic beats over the period. Of these, 18,000 are monomorphic ventricular ectopics, mostly in bigeminy and trigeminy. There is no ventricular tachycardia or atrial fibrillation.
Q4. What is the significance of this report and what should be done next?
Shayla needs urgent cardiac echocardiography. Studies suggest that up to 100 ventricular ectopic beats in a 24-hour period on Holter monitoring are within normal limits.3 Ventricular ectopics that number more than 15,000 in 24 hours on Holter monitoring in patients without underlying heart disease can cause such frequent and irregular contractions of the ventricle that ventricular dysfunction or dilated cardiomyopathy may develop.2,3 Older patients and those with underlying cardiac disease, in particular, are at risk of these complications. The number of ectopic beats that Shayla has may result in shortness of breath, chest discomfort and feeling faint and nonspecifically unwell.
Monomorphic ventricular ectopic beats signify a specific abnormal focus of electrical activity in the myocardium and are a risk factor for ventricular tachycardia and ventricular fibrillation. They are also a marker of increased all-cause mortality.3
Q5. What is the differential diagnosis at this stage?
The greatest concern is that Shayla had myocarditis (plus viral pneumonitis with bacterial complications) due to the illness six weeks ago and that she now has virally induced cardiomyopathy. This needs to be excluded. Shayla is also potentially at risk of ventricular tachycardia and ventricular fibrillation because of the extreme number of monomorphic ventricular ectopic beats. Pericarditis is another possible consequence of the viral infection six weeks ago and could cause shortness of breath.
It is also possible that Shayla did not have viral myocarditis, but just a bacterial complication of viral pneumonitis. The condition may have been exacerbated by her severe stress coping with grief and also overworking.
Her serum IgG immunity to SARS-CoV-2 is due to previous exposure to the virus. Reinfection is definitely possible. However, the illness is unlikely to have been COVID-19 because of the negative results for IgM and on PCR testing, which is more sensitive than rapid antigen testing.
Cardiac echocardiography has normal results. There is no evidence of pericarditis (fluid within the pericardium). The cardiologist then performs a plain exercise stress test.
Q6. Why does the cardiologist perform an exercise stress test?
Ventricular ectopic beats that are not likely to be pathological tend to be abolished with significant exercise and to return in the phase immediately after exercise. The exercise stress test may also identify underlying myocardial ischaemia, although it is not as accurate as cardiac stress echocardiography.
Outcome
Shayla undergoes an exercise stress test, and the ventricular ectopic beats are abolished. There are no ischaemic changes, but she is short of breath during the test; the cardiologist feels this is mainly due to her being currently unfit. The ectopic beats return after exercise.
Shayla recalls having 24-hour Holter monitoring and cardiac echocardiography 10 years previously when she was extremely stressed during her divorce. The Holter monitoring showed many multifocal ectopic beats, but not considered enough to treat with medication. She does not recall any shortness of breath at the time. Cardiac echocardiography was normal. Her condition settled over weeks.
Shayla is now treated with flecainide 50 mg twice daily, digoxin 62.5mcg daily and a magnesium supplement once daily. Although flecainide is pro-arrhythmic, it is unlikely to have this effect at a low dose in a structurally normal heart. Metoprolol or another beta blocker is not used, as Shayla is usually very active, and the cardiologist does not want to cause bradycardia or hypotension during exercise. The cardiologist feels her extreme levels of stress are the most likely cause of the multiple ectopic beats and hence her shortness of breath, similar to her presentation 10 years previously.
Shayla’s shortness of breath disappears within two days of starting this treatment. The cardiologist organises repeat 24-hour Holter monitoring in three months’ time to confirm the ventricular ectopic beats have settled on medication. If so, the cardiologist plans to cease treatment when Shayla is less stressed and to repeat 24-hour Holter monitoring off medication. If she has no recurrence, she can choose to cease the medication permanently. Electrophysiological catheter ablation could be considered if her condition does not respond satisfactorily to medication. CT
COMPETING INTERESTS: None.