Takotsubo syndrome. What becomes of the broken hearted?
Often considered to run a benign and self-limiting course, the darker prognosis of takotsubo cardiomyopathy is increasingly being recognised, with up to a quarter of affected patients having severe clinical complications. Early diagnosis requires excluding acute coronary syndromes, and recognition of high-risk prognostic features may help to minimise morbidity and mortality.
- Takotsubo syndrome (TTS) is a transient cardiomyopathy provoked by catecholamine surge.
- A triggering stressful event, which may be emotional, physical or psychological, is present in two-thirds of patients with TTS.
- Postmenopausal women comprise 90% of patient with TTS.
- TTS presents as an acute coronary syndrome mimic and diagnosis requires exclusion of coronary disease.
- Risk factors for poor outcomes from TTS include older age, physical stress as a trigger and atypical patterns of left ventricular dysfunction.
- The inhospitable rate of serious complications is about 20% and the risk of inhospitable death is 1.8%.
- Management is predominantly supportive until cardiac dysfunction improves.
- Observational data indicate treatment with ACE inhibitors and angiotensin receptor blockers may improve survival at one year.
- TTS has a recurrence rate of 1%.
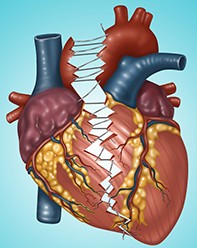
Takotsubo syndrome (TTS), also known as takotsubo cardiomyopathy, stress cardiomyopathy or broken heart syndrome, was first described in a case series published in a Japanese medical textbook in 1990,1 and first described in Caucasian patients in 1997.2 TTS is an acute and transient impairment of left ventricular systolic function, named for the resemblance of the shape of the left ventricle in systole to a Japanese octopus trap (Figure 1).
The condition is thought to be triggered by a catecholaminergic surge associated with physical, psychological or emotional stressors. Patients often spontaneously recover within days or weeks. Although most cases are relatively benign and self-limiting, up to 25% of affected patients may suffer severe clinical complications. Supportive management is required in the acute phase; however, limited data are available to guide ongoing treatment after the index episode.
Epidemiology
Once thought to be a rare disease, increased awareness of TTS has led to it being recognised as the underlying abnormality in around 1 to 2% of all patients presenting with a suspected acute coronary syndrome (ACS).3 Current data from TTS registries in Europe and the USA report an incidence of 15 to 30 cases per 100,000 population annually. The true incidence is likely to be much higher, as it would include milder cases that did not come to medical attention.
Clinical features
The most common presenting symptoms of TTS are dyspnoea and chest pain, mimicking an ACS and occurring within minutes to days after a triggering stressor. If the left ventricular function is severely impaired or left ventricular outflow tract obstruction (LVOTO) occurs, initial presentation may be with acute pulmonary oedema, syncope, cardiogenic shock, ventricular arrhythmia or cardiac arrest.4 More than 90% of affected patients are postmenopausal women, with a mean age of 65 to 70 years (Figure 2).5,6
Triggers are present in about two-thirds of affected patients, most often emotional stressors such as bereavement or relationship breakdown, psychological stressors such as extreme fear or danger, or physical stressors such as surgery or exacerbation of chronic obstructive pulmonary disease or asthma. However, up to 35% of cases are not preceded by a stressful triggering event.7 Acute intracerebral events associated with a catecholamine surge, such as brain trauma, subarachnoid haemorrhage or seizures, have also been associated with TTS (termed neurogenic myocardial stunning). Diabetes is present in 10 to 25% of patients with TTS, supporting an aetiological role of microvascular dysfunction and endothelial dysregulation.
Pathophysiology
The exact pathophysiology of takotsubo cardiomyopathy is incompletely understood – for example, why stressors lead to myocardial dysfunction in some cases and not in others, why the syndrome is typically not recurrent despite recurrent exposures to stressful situations, and why one-third of cases do not have a clear associated triggering event.
Animal studies support a theory of catecholamine-related myocardial injury as the underlying cause of TTS. Exposure of a predisposed person to a stressful stimulus triggers a cascade of central nervous system signalling, converging on the hypothalamus and activating the hypothalamic-pituitary-adrenal axis and sympathetic nervous system. This in turn leads to both adrenal secretion of catecholamines into the systemic circulation and local downstream release of noradrenaline and neuropeptide Y stored in presynaptic terminals of sympathetic neurons converging directly on the myocardium.3
Spillover of these adrenergic molecules may cause direct myocardial toxicity through microvascular dysfunction and localised coronary spasm, producing a demand-supply imbalance and consequent ischaemic myocardial injury. People who are predisposed to TTS may have enriched stores of adrenaline and neuropeptide Y within presynaptic terminal granules, with a larger release and spillover on exposure to stressful stimuli. The pattern of ventricular hypokinesis produced by the catecholaminergic surge is thought to relate to the distribution of adrenergic receptors on ventricular myocardium, being more densely located in the apical segments of the ventricular myocardium and less dense in the basal segments.8
An increase in systemic circulating catecholamines is also proposed to contribute to the pathophysiology of the cardiomyopathy and is the mechanism of cardiac injury in conditions of systemic catecholamine excess such as phaeochromocytoma. Although typical TTS is usually related to an acute and self-limited adrenergic activation, the cardiomyopathy in phaeochromocytoma often results from prolonged exposure to supraphysiological catecholamine levels, leading to myocardial fibrosis seen on cardiac MRI that is not seen in typical TTS.9
Autopsy studies and endomyocardial biopsies from affected patients show focal myocytolysis, mononuclear lymphocytic infiltration and ‘contraction band necrosis’. Contraction band necrosis describes hypercontracted myofilaments thought to be related to catecholamine-induced severe calcium overload with cardiomyocytes; and is also seen in the myocardium of individuals that died in terrifying circumstances such as acute severe asthma attack or physical assault.10
The predisposition to adrenergic-induced myocardial toxicity among the group most affected by TTS, postmenopausal women, may be due to loss of the vasomotor regulatory effects of oestrogen and an increased prevalence of anxiety and depression. These conditions lead to increased stores of catecholamines within neuronal terminals and an increased frequency of risk factors for microvascular dysfunction such as diabetes and hypertension (Figure 3).7
Diagnosis
Patients presenting with TTS are often clinically indistinguishable from those presenting with an ACS. Echocardiography and coronary imaging (either CT coronary angiography or invasive angiography) are required to make the diagnosis.4
Results of biochemical investigations are notable for a mildly elevated troponin level with significantly elevated brain natriuretic peptide or N-terminal pro b-type natriuretic peptide. An initial electrocardiogram may show changes such as T-wave inversion (41%), ST-segment elevation (44%) or ST-segment depression (8%) that extend beyond a single coronary territory, and this may be followed by development of T-wave inversion and/or QT prolongation that subsequently resolves over days to weeks.4 Pulmonary congestion or alveolar oedema may be seen on chest x-ray.
A transthoracic echocardiogram characteristically shows left ventricular regional wall motion abnormalities extending beyond the distribution of a single epicardial coronary artery territory. The classic pattern of apical ballooning occurs as a result of hypokinesis or akinesis of the entire apical myocardium, with relative basal segment hyperkinesis.3 This pattern occurs in 75 to 80% of patients with TTS and may be associated with left ventricular outflow tract obstruction and consequent cardiogenic shock or ventricular arrhythmia due to vigorous basal segment contraction and reduced cardiac output, and mitral regurgitation due to systolic anterior motion of the mitral valve. The other 20% of patients have other patterns of left ventricular systolic dysfunction – such as midventricular hypokinesis in 10 to 20%, basal hypokinesis (‘reverse’ TTS) in 5%, or, rarely, focal segmental hypokinesis. The midventricular pattern of TTS, in which the mid ventricle is hypokinetic or akinetic, is more frequently associated with severe left ventricular dysfunction, more severe reduction in cardiac output and cardiogenic shock (Figure 4).
Coronary angiography is required to exclude epicardial coronary stenosis as the cause of symptoms and ventricular dysfunction. Given the average age at presentation of 70 to 75 years, it is not uncommon to find so-called ‘bystander’ coronary disease on angiography; however, the extension of hypokinesis beyond a single coronary territory on the echocardiogram signifies TTS as the likely primary clinical pathology.
Diagnostic criteria were proposed in 2016 by the International Takotsubo (InterTAK) Registry, building on the Mayo Clinic Diagnostic Criteria of 2008 (Box).11,12
The InterTAK Diagnostic Score quantifies the clinical probability of TTS and helps to distinguish between TTS and ACS. It can be used to guide investigations.13 The criteria and corresponding point score are as follows:
• female sex, 25 points
• emotional trigger, 24 points
• physical trigger, 13 points
• absence of ST-segment depression, 12 points
• psychiatric disorders, 11 points
• neurological disorders, 9 points
• QTc prolongation, 6 points.
Patients with a score greater than 70 have a 90% probability of TTS being the underlying diagnosis.
Management
In the acute setting, the management of TTS and its complications is predominantly supportive. Patients presenting in cardiogenic shock should be evaluated for LVOTO either with transthoracic echocardiography or with a left ventricular-to-aortic pullback measured at the time of coronary angiography. Catecholaminergic inotropes and vasopressors should be avoided, as a 20% mortality rate has been reported with the use of these agents in acute TTS; however, the intracellular calcium sensitiser levosimendan appears to be a safe alternative in this setting (available in Australia under the TGA Special Access Scheme).14 Mechanical circulatory support devices such as the Impella ventricular support system, intra-aortic balloon pump and left ventricular assist device may also be considered in cases of acute refractory cardiogenic shock for temporary haemodynamic support.15 Beta blockers can be used to relieve LVOTO but cannot be used in cases of severely impaired left-ventricular systolic function, hypotension, QTc prolongation greater than 500 milliseconds or bradycardia.
Cardiac monitoring should be performed for 48 hours for all patients with primary TTS. Tachyarrhythmias and bradyarrhythmias should be managed using standard protocols, and special attention must be given to QTc monitoring and avoiding QT-prolonging drugs. Because of the transient nature of TTS and associated rhythm abnormalities, temporary pacing methods such as transvenous temporary pacing wire or temporary-permanent transvenous pacing should be utilised, as opposed to implantation of permanent devices. External wearable cardiac defibrillators could be considered in patients with persistently impaired LV function or ventricular tachyarrhythmia, although these have not been studied in this population and have not been shown to prevent arrhythmic death in early ischaemic ventricular dysfunction.16
Treatment for pulmonary oedema and acute heart failure includes diuretics and nitrates; however, these drugs should be avoided in patients with LVOTO as they reduce preload, worsening the obstruction to LV ejection, and thus reduce cardiac output. Anticoagulation may be considered for prevention of left ventricular thrombus and subsequent arterial thromboembolism in cases of severe apical hypo- or akinesis, or if the LV ejection fraction is less than 30%.4 The use of ACE inhibitors and angiotensin receptor blockers (ARBs) has been shown in an observational study of 1750 patients to be associated with improved survival at one year after the index presentation.6 There was no survival benefit from beta blockers over the same period. ACE inhibitors or ARBs are thus recommended in the acute setting to facilitate left ventricular recovery and improve mortality outcomes at one year; however, there have been no studies assessing the optimal duration of ongoing ACE inhibitor/ARB therapy after acute TTS. These drugs should be continued in any patient with recurrent TTS.
Prognosis
TTS was originally thought to have a good long-term outcome after the index episode. It is increasingly recognised that TTS has a wide clinical heterogeneity ranging from a benign course with rapid recovery to a fulminant course with severe cardiac dysfunction, heart failure and death. In the acute phase, haemodynamic and electrical instability are the drivers of inhospital morbidity and mortality and occur in up to 20% of patients with TTS.4
A meta-analysis of 54 studies published in 2019 analysed the outcomes and overall prognosis of TTS in more than 4600 patients and reported a darker prognosis for TTS than previously thought, emphasising the potential seriousness of the condition and highlighting prognostic markers for poor outcomes.17 In this meta-analysis, frequency of serious complications was high, including acute heart failure with shock in 19% of patients, malignant arrhythmias in 10% and inhospital death in 1.8%. Late death (more than six months after admission over a median follow-up period of 28 months) occurred in 10.2% of the total population, although only one-quarter of these deaths were from cardiac causes, equating to an annual mortality rate of 3.5%. Long-term mortality was significantly associated with older age, a physical stressor as the trigger (secondary form of TTS) and an atypical pattern of left ventricular hypokinesis, but was not associated with acute heart failure at presentation or cardiogenic shock. The annual recurrence rate for TTS was 1.0%, and recurrence was not predicted by the severity of the initial presentation.
The long-term rates of mortality and recurrence are therefore not trivial and patients with any of the presenting features that predict a poorer long-term prognosis should be followed up closely.
Conclusion
Takotsubo cardiomyopathy is a common condition mimicking an ACS that has a diverse clinical course and high rates of morbidity and mortality. Early diagnosis to exclude coronary disease, recognition of patients at higher risk for complications and death, initiation of appropriate supportive care and commencement of ACE inhibitors or ARBs are central in management. CT