A young girl with Turner syndrome and an abnormal ECG
Articles in this section are inspired by, but not based on, real cases to illustrate the importance of knowledge about ECGs in relation to clinical situations in general practice. Management is not discussed in detail.
- Incomplete right bundle branch block is seen in 3% of children and is of no clinical significance if the child is healthy with no other abnormalities; in these cases, it does not need further cardiac investigation.
- In healthy adults, incomplete right bundle branch block carries no concerning prognosis but may need further investigation if the patient has cardiac or pulmonary risk factors.
- Patients with complete right bundle branch block require referral to a cardiologist for further investigation if there are abnormalities on physical examination or if the history suggests a likelihood of coronary artery disease, other electrophysiological abnormalities or valve disease.
- Patients with Turner syndrome have a 50% chance of congenital heart disease.
- Patients with Turner syndrome have a reduced life expectancy because of an increased risk of stroke, early onset hypertension, early onset ischaemic heart disease and obesity and its metabolic consequences.
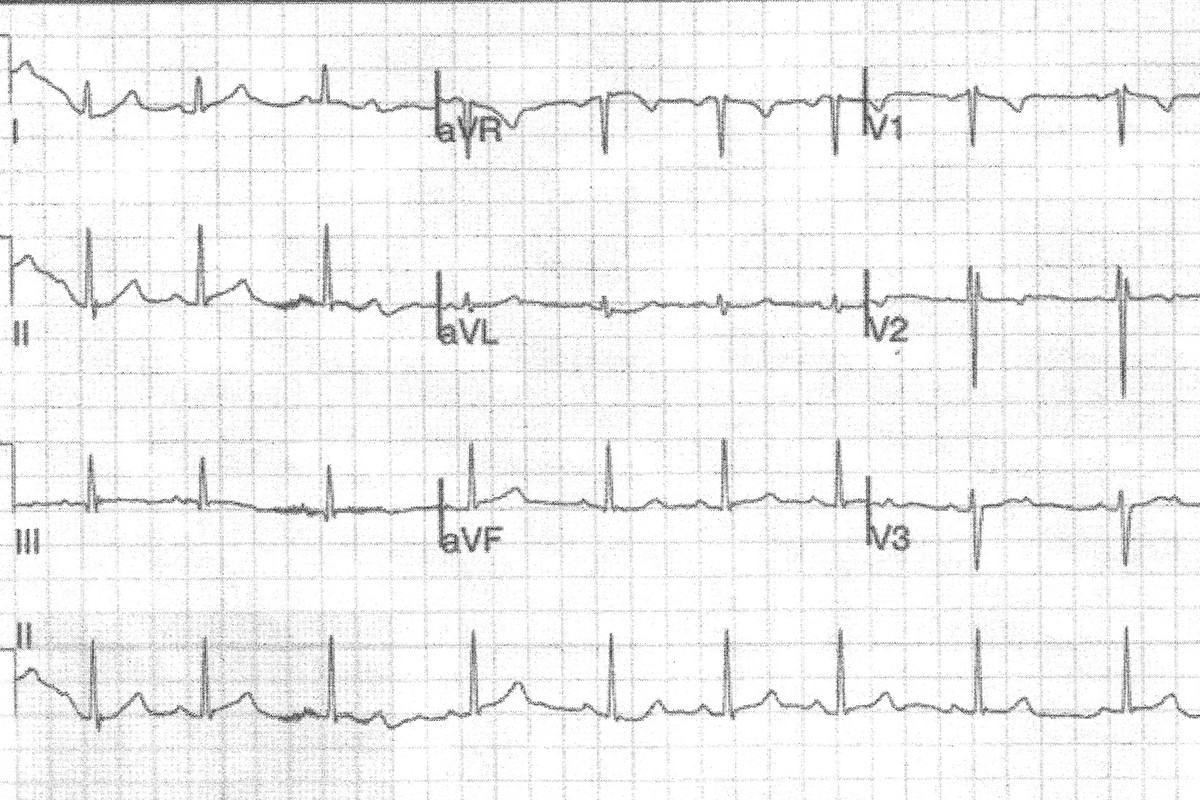
Arna, aged 5 years, is a patient at your practice. Her parents present with concern about her growth as she has just started school, and they have noticed she is one of the shortest children in her school year, despite both of them being of normal stature. You refer Arna to a paediatrician who diagnoses Turner syndrome. She undergoes baseline cardiac investigations, including an ECG (Figure).
Q1. What does this ECG show?
The ECG shows sinus arrhythmia with incomplete right bundle branch block, indicated by an RSR’′pattern in the V1 and V2 leads.
Q2. How significant is incomplete right bundle branch block on a paediatric ECG?
Incomplete right bundle branch block is seen in 3% of the paediatric population, especially in younger children.1 It is considered to be of no clinical significance if the child is healthy with no other abnormalities and, by itself, does not need further cardiac investigation. In patients with Turner syndrome, incomplete right bundle branch block is more common, found in 23% of patients in one study.1
It should be noted that ECG changes are not diagnostic of any cardiac abnormalities in Turner syndrome, and echocardiography is always needed to assess the child.
Q3. What causes a right bundle branch block pattern on an ECG?
Depolarisation travels from the left ventricle to the right ventricle across the septum. In the presence of a right bundle branch block, the left bundle branch depolarises normally, but the right bundle branch does not. The electrical impulse is slowed in the right ventricle, as may be reflected as an RSR’ (M-shaped) pattern in the right precordial leads (V1, V2 and V3) and slurring and widening of the S wave in the lateral leads (I, aVL, V5 and V6). The secondary repolarisation is abnormal, and so there are also ST abnormalities and T-wave inversion in the right precordial leads (V1 to V3). Because the electrical impulse travels normally through the left side of the heart and the septum, the early section of the QRS complex in the left precordial leads (V5 and V6) appears normal. The axis is normal if the right bundle branch block is not associated with any other electrophysiological abnormalities.
In a complete right bundle branch block, the QRS duration is 120ms or longer. An incomplete right bundle branch block is diagnosed when the QRS duration is 110ms or longer but less than 120ms in adults and 80ms to 100ms in children.
Q4. How significant is incomplete right bundle branch block in adults?
Incomplete right bundle branch block is not uncommonly seen in adults (3% to 7%), and is more common in men and athletes.2 If the patient has abnormal results on cardiac examination, cardiac symptoms or risk factors for cardiac or pulmonary disease, they should be further investigated.
By itself, in an otherwise healthy adult, incomplete right bundle branch block carries no concerning prognosis. This contrasts with complete right bundle branch block, in which case the patient should always have a history taken and a thorough physical examination. However, if there is any concern about other electrophysiological abnormalities, coronary artery disease, valvular disease or pulmonary disease in a patient with incomplete or complete right bundle branch block, the patient should be referred to a cardiologist for further investigation.
Q5. What cardiac conditions are associated with Turner syndrome?
About 50% of patients with Turner syndrome have congenital heart abnormalities.3 There is some correlation between the severity of the karyotype abnormality (nonmosaic 45X karyotype versus other karyotypes) and the presence and severity of congenital cardiac disease.1
Congenital abnormalities commonly associated with Turner syndrome include bicuspid aortic valve, aortic valve stenosis (usually mild), aortic coarctation, partial anomalous pulmonary venous return and hypoplastic left heart syndrome. Patients with Turner syndrome also have a tendency to aortic dilation and aortic dissection, especially if they have congenital heart disease, but also as they commonly develop early-onset hypertension and are prone to obesity and its metabolic complications.3 Women with Turner syndrome also have a higher incidence of stroke and early ischaemic heart disease. These factors account for a life expectancy about 10 years less than average.3
Q6. How is aortic coarctation tested for at the neonatal six-week check?
The most common site for coarctation of the aorta is just beyond the left subclavian artery, in the region of a patent ductus arteriosus or the ductal ligamentum. However, narrowing can occur anywhere along the aortic arch, the thoracic aorta and, rarely, the abdominal aorta.
Cardiac auscultation may suggest a systolic murmur loudest along the left shoulder blade or interscapular region posteriorly, in the left axilla and in the upper left sternal border anteriorly. There may be a soft bruit over the affected region if there is coarctation of the abdominal aorta. If a bicuspid aortic valve is present there may be an apical systolic ejection click.
In addition to auscultation, in every neonate the doctor should place one index finger on the baby’s brachial pulse and another index finger on the femoral pulse and compare the two. A delay in the femoral pulse or a weaker femoral pulse are significant findings. It should be noted that this test is very sensitive if findings are abnormal, but normal findings do not exclude coarctation of the aorta.
Additional findings suggesting coarctation of the aorta include a higher blood pressure (or hypertension) in the upper limbs compared with the lower limbs.
Outcome
Echocardiography shows that Arna has a bicuspid aortic valve with mild aortic stenosis. The ejection fraction is normal, with no ventricular hypertrophy, no coarctation of the aorta and normal pulmonary artery pressure. Her thyroid function is normal (patients with Turner syndrome are prone to hyperthyroidism and hypothyroidism).
Arna will have annual echocardiography and careful blood pressure observation and will need good dental care. Her parents have been told to monitor her exercise tolerance, as aortic stenosis can cause faintness and poor stamina. Arna’s bicuspid aortic valve pathology may slowly worsen with age. CT
COMPETING INTERESTS: None.
References