Managing cardiac-related mental health problems: challenges and solutions

Postcardiac event mental health issues are common and can compromise recovery. A patient-centred and collaborative approach to the overall management of postcardiac event mental health problems will optimise the emotional recovery of cardiac patients.
- Anxiety and depression are common after cardiac events and compromise recovery.
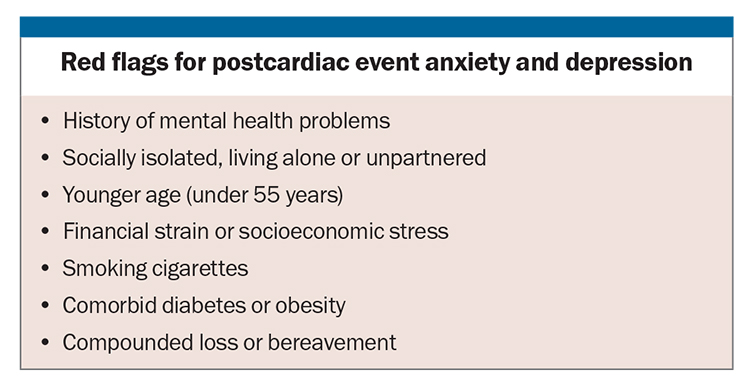
- Risk factors for postcardiac event anxiety and depression include a history of mental health problems, social isolation, financial strain, younger age (under 55 years), smoking, comorbid diabetes or obesity, and compounded loss or bereavement.
- General practice provides an ideal setting for patient education, screening, treatment and referral to manage postcardiac event mental health issues.
- Interdisciplinary collaborative care has been shown to optimise patients’ mental and physical recovery.
The mental health impact of coronary heart disease has gained increasing research attention in the past two decades. There is now considerable consensus that postcardiac event mental health issues are common and can compromise recovery. There is somewhat less agreement on how and when these issues should be managed and by whom. Given the prognostic importance of postcardiac event mental health problems, it is imperative that its identification and management is approached in a systematic and collaborative way.
Nature of psychosocial impacts of cardiac events
Cardiac events, such as acute coronary syndrome (ACS), acute myocardial infarction (AMI), cardiac arrest and spontaneous coronary artery dissection (SCAD), trigger a broad range of psychosocial challenges for patients, which can include shock, uncertainty, confusion and vulnerability.1,2 These feelings are heightened in young patients and individuals who experience unexpected events, such as SCAD.2,3 After a cardiac event, patients typically fear recurrence or sudden death, and worry about adjusting to a challenging and possibly foreshortened future.1-4 Loss of independence and control, and changes in self-identity and roles are common, including negative impacts on work capacity, personal relationships, social life and exercise regimens.1,2 These fears and losses also occur after procedures such as coronary artery bypass graft surgery, percutaneous coronary intervention and implantable cardioverter defibrillator surgery.1 Physical symptoms of fatigue, breathlessness and pain add to the patients’ distress and frustration, whereas rigorous medication regimens and recommended lifestyle changes challenge patients’ sense of identity and autonomy, often exacerbating feelings of sadness, helplessness and hopelessness.1,2,5 Some patients go on to experience clinically significant postcardiac event anxiety and depression, both of which impact negatively on recovery and prognosis.6,7
Prevalence of postcardiac event anxiety and depression
About one in three patients experience clinically significant anxiety and about one in four become depressed after AMI, cardiac arrest, coronary artery bypass graft surgery or percutaneous coronary intervention, rates that are twice those seen in the general population.7-11 Rates of anxiety, in particular, are even higher following SCAD.12 Post-traumatic stress disorder is also common, varying from 15% to 20% in patients with ACS, and up to 35% in patients after cardiac arrest and implantable cardioverter defibrillator surgery.13,14 Compared with the general population, ACS and other cardiac diagnoses are associated with a 50% increased risk of suicide, increasing to an almost fivefold increased suicide risk following cardiac arrest.15
Predictors of postcardiac event anxiety and depression
The past often predicts the future, and postcardiac event mental health status is no exception: patients with a history of pre-event mental health problems have a fourfold increased risk of postevent anxiety or depression.7,16,17 Social connectedness is also important: those who are socially isolated, living alone or unpartnered have a twofold increased risk of postcardiac event mental health problems.7,8,16,18 Other risk factors or ‘mental health red flags’ include being younger (aged under 55 years), being under financial strain or socioeconomic stress, smoking cigarettes, having comorbid diabetes or obesity and experiencing compounded loss or bereavement (see Box).7,11,16-19 Indeed, the risk of first or subsequent cardiac events increases in the aftermath of bereavement.20,21
Consequences of postcardiac event anxiety and depression
Postcardiac event mental health problems negatively impact prognosis, increasing the risk of hospital readmission, recurrent cardiac events and premature mortality.22-24 This is not surprising, as anxiety and depression compromise health-enhancing behaviours, such as medication adherence, engaging in physical activity, dietary changes, smoking cessation and cardiac rehabilitation attendance.24-28 Postcardiac event anxiety and depression are also associated with increased inflammation, altered autonomic function and poor functional capacity,29,30 highlighting the shared mechanisms between heart disease and mental illness.
Opportunities for screening, education and treatment
Over the course of a patient’s cardiac journey, there are numerous opportunities for mental health screening, education and treatment. These include the preadmission period, period of hospitalisation, and immediate and later postcardiac event periods.
Screening
Australian cardiac guidelines recommend routine mental health screening at the time of the acute cardiac event, at first follow up, at two to three months postcardiac event, and subsequently on a yearly basis.31 Ideally, every opportunity should be utilised to monitor mental health symptoms. Recommended screening tools include the Generalised Anxiety Disorder (GAD-7) for anxiety and the Patient Health Questionnaire (PHQ-9) for depression.24,31,32 The importance of communication and collaboration between healthcare professionals cannot be over stated: screening results should be documented in the patient’s medical record and communicated to others involved in the patient’s care. The value of screening is limited unless adequate systems are in place to ensure accurate diagnosis, effective communication, appropriate referral and follow up, and effective treatment.32
Patient education
Patients need to be given a clear explanation about the likelihood, risk factors and consequences of postcardiac event anxiety and depression, with reference to their own personal circumstances and red flags for mental health problems.16 Patients without mental health red flags can be reassured that they are unlikely to develop postcardiac event problems, whereas those who are younger (aged under 55 years), have a mental health history, live alone or have comorbid conditions, can be alerted to their increased mental health risk. Evidence shows that cardiac patients want to know about postcardiac event mental health risks and feel grateful for the opportunity to discuss these issues with a trusted healthcare professional.33
Mood difficulties are often heightened during the initial two- to three-month adjustment period, yet resolve without intervention for many patients.34 These transient symptoms are referred to as the ‘cardiac blues’ and are likened to a bereavement or adjustment response.6,35 During this early postcardiac event period, symptoms need to be acknowledged but not necessarily pathologised, to allow time for adjustment and natural resolution. Patients with elevated anxiety or depressive symptoms should be closely monitored with repeat screening and referral for mental health support as required.6,36,37
Treatment
The recommended mental health treatments for cardiac patients include cardiac rehabilitation attendance, lifestyle changes, psychological interventions, pharmacological treatments and collaborative care.31 Cardiac rehabilitation attendance decreases morbidity and improves quality of life and survival.38-40 Physical activity and exercise significantly improve postcardiac event anxiety and depression and reduce morbidity and premature mortality because of their effects on enhancing parasympathetic tone and decreasing inflammation, with benefits equivalent to the use of pharmacological treatment.41-43 In terms of psychological therapies, cognitive behaviour therapy is recommended in Australian clinical cardiac guidelines for mental health management,31 which results in reduced mental health symptoms and, in some studies, reduced mortality risk.24,44-49 There is also convincing evidence that the use of pharmacological treatments, most notably selective serotonin reuptake inhibitors, result in reduced anxiety, depression and AMI recurrence in cardiac patients.24,48,50 Pharmacological and psychological interventions can be combined for enhanced outcomes.44 However, interactions between certain selective serotonin reuptake inhibitors and antihypertensive medications have been reported.51 Moreover, there is some concern with the use of serotonin and norepinephrine reuptake inhibitors in cardiac patients due to the risk of cardiovascular side effects, including elevated blood pressure and bleeding.52 Finally, collaborative care has also been shown to be effective and allows cardiac and mental health issues to be managed concurrently.53
Sharing the responsibility through collaborative mental health management
Cardiac patient care is shared between cardiologists and cardiac surgeons, GPs and the cardiac rehabilitation team of allied healthcare professionals. For some patients, referral to a psychologist or psychiatrist is warranted. Although barriers exist in each setting, taking a shared, collaborative and interdisciplinary approach to the identification and management of postcardiac event mental health problems is likely to result in optimal patient care.31,53 Indeed, the 2023 statement of the Association of Cardiovascular Nursing and Allied Professions of the European Society of Cardiology recommended an integrated, interdisciplinary approach to achieve optimal cardiovascular care more generally,54 whereas the recently released 2023 guidelines from the American Heart Association and the American College of Cardiology joint committee highlight the importance of incorporating the principles of shared decision-making and team-based care in the management of cardiac patients.24
Cardiologists currently play only a modest role in managing cardiac mental health. A recent study of 524 cardiologist members of the Cardiac Society of Australia and New Zealand found that only 3% routinely screen for depression, with most only ‘sometimes’ asking patients about their mood.55 Consistently, only a minority routinely refer their patients with depression for treatment or prescribe antidepressant medication, with the majority lacking confidence in prescribing depression treatment. Currently, most cardiologists regard GPs as being primarily responsible for both identifying and managing cardiac-related depression.55 Regardless, given that the opinions of cardiologists are highly valued by patients, it is important that cardiologists be supported to take an active role in mental health identification and management.
GPs are well placed to screen, monitor, treat and refer cardiac patients with mental health problems. In Australia, GPs are the most commonly consulted healthcare professional, even for mental health issues.56 Almost all (95%) Australians with a chronic condition consulted a GP during 2022.56 However, there is currently a lack of consistency in anxiety and depression screening and identification in the acute inpatient setting,57 due to time limitations and the lack of remuneration.32 Indeed, the burden of mental health management is falling increasingly, overwhelmingly and disproportionately to GPs and primary care physicians, who often feel inadequately equipped to manage these conditions,58 further highlighting the need for interdisciplinary, shared-care models.
Outpatient cardiac rehabilitation programs provide an ideal opportunity for routine and repeat screening for anxiety and depression. A recent Australian study identified reasonably high rates of screening on both entry to and exit from cardiac rehabilitation.59 However, screening efforts in this setting are compromised by suboptimal cardiac rehabilitation attendance60 and tendencies towards underscreening of patients undergoing cardiac rehabilitation who are most in need of support, such as young patients, those with comorbidities, smokers, those of lower socioeconomic status and those who are less physically active.61 Although cardiologists are more likely than primary care physicians to refer patients to cardiac rehabilitation programs,62 both should be encouraged and supported to routinely refer cardiac patients to cardiac rehabilitation.
All primary care physicians and cardiologists have a central role in the referral of patients to specialist psychological and psychiatric services when warranted. It is therefore imperative for GPs, cardiac specialists and cardiac rehabilitation practitioners to know their referral options, including locally based psychologists and psychiatrists, and other relevant services. For example, the Cardiac Counselling Clinic of the Australian Centre for Heart Health offers evidence-based, cardiac-specific counselling and support through its team of trained registered psychologists.
Summary
Clearly, challenges and gaps exist at each opportunity and in each setting. This highlights the need for a systematic effort across the entire patient journey, with increased interdisciplinary communication and collaboration. Ideally, every patient encounter in each setting should be viewed as an opportunity for mental health education, screening, treatment and referral. Taking a patient-centred and collaborative approach to the overall management of postcardiac event mental health problems will optimise cardiac patients’ emotional recovery. CT
COMPETING INTERESTS: None.
References
1. Jackson AC, Rogerson MC, Amerena J, et al. Unraveling the complexity of cardiac distress: a study of prevalence and severity. Front Psychiatry 2022; 13: 808904.
2. Murphy B, Rogerson M, Hesselson S, et al. Psychosocial impacts of spontaneous coronary artery dissection: a qualitative study. PloS One 2022; 17: e0273978.
3. Merritt CJ, de Zoysa N and Hutton JM. A qualitative study of younger men’s experience of heart attack (myocardial infarction). Br J Health Psychol 2017; 22: 589-608.
4. Doiron-Maillet N and Meagher-Stewart D. The uncertain journey: women’s experiences following a myocardial infarction. Can J Cardiovasc Nurs 2003; 13: 14-23.
5. Simonÿ CP, Dreyer P, Pedersen BD, et al. It is not just a minor thing - a phenomenological-hermeneutic study of patients’ experiences when afflicted by a minor heart attack and participating in cardiac rehabilitation. Scand J Caring Sci 2017; 31: 232-240.
6. Murphy B, Higgins R, Jackson A. Anxiety, depression and psychological adjustment after an acute cardiac event. In: Byrne D and Alvarenga M (eds) Handbook of Psychocardiology. Singapore: Springer, 2016.
7. Murphy B, Le Grande M, Alvarenga M, et al. Anxiety and depression after a cardiac event: prevalence and predictors. Front Psychol 2019; 10: 3010.
8. Khan Z, Musa K, Abumedian M, et al. Prevalence of depression in patients with post-acute coronary syndrome and the role of cardiac rehabilitation in reducing the risk of depression: a systematic review. Cureus 2021; 13: e20851.
9. Pogosova N, Kotseva K, De Bacquer D, et al. Psychosocial risk factors in relation to other cardiovascular risk factors in coronary heart disease: Results from the EUROASPIRE IV survey. A registry from the European Society of Cardiology. Eur J Prev Cardiol 2017; 24: 1371-1380.
10. Yaow CYL, Teoh SE, Lim WS, et al. Prevalence of anxiety, depression, and post-traumatic stress disorder after cardiac arrest: A systematic review and meta-analysis. Resuscitation 2022; 170: 82-91.
11. Rawashdeh SI, Ibdah R, Kheirallah KA, et al. Prevalence estimates, severity, and risk factors of depressive symptoms among coronary artery disease patients after ten days of percutaneous coronary intervention. Clin Pract Epidemiol Ment Health 2021; 17: 103-113.
12. Murphy BM, Rogerson MC, Hesselson S, et al. Prevalence of anxiety, depression, and distress in SCAD and Non-SCAD AMI patients: a comparative study. J Cardiopulm Rehabil Prev 2023; 43: 338–345.
13. Vilchinsky N, Ginzburg K, Fait K, et al. Cardiac-disease-induced PTSD (CDI-PTSD): A systematic review. Clin Psychol Rev 2017; 55: 92-106.
14. Tulloch H, Greenman PS, Tassé V. Post-traumatic stress disorder among cardiac patients: prevalence, risk factors, and considerations for assessment and treatment. Behav Sci 2015; 5: 27-40.
15. Petersen BD, Stenager E, Mogensen CB, et al. The association between heart diseases and suicide: a nationwide cohort study. J Intern Med 2020; 287: 558-568.
16. Murphy BM, Elliott PC, Ludeman D, et al. ‘Red flags’ for anxiety and depression after an acute cardiac event: 6-month longitudinal study in regional and rural Victoria. Eur J Prev Cardiol 2014; 21: 1079-1089.
17. Sever S, Harrison AS, Doherty P. Levels of depressive symptoms in cardiac patients attending cardiac rehabilitation with a history of depression: pre Covid-19 and Covid-19 period comparison. BMC Cardiovascular Disorders 2022; 22: 427.
18. Pogosova N, Boytsov S, De Bacquer D, et al. Factors associated with anxiety and depressive symptoms in 2775 patients with arterial hypertension and coronary heart disease: results from the COMETA Multicenter Study. Glob Heart 2021; 16: 73.
19. Bruyninx G, Grenier J, Greenman PS, et al. Prevalence of symptoms of anxiety disorders and depression in cardiac rehabilitation patients in an academic hospital: a case study. Psychiatric Quarterly 2021; 92: 273-287.
20. Carey IM, Shah SM, DeWilde S, et al. Increased risk of acute cardiovascular events after partner bereavement: a matched cohort study. JAMA Intern Med 2014; 174: 598-605.
21. Wei D, Janszky I, Ljung R, et al. Bereavement and prognosis after a first acute myocardial infarction: a swedish register‐based cohort study. J Am Heart Assoc 2022; 11: e027143.
22. Worcester MU, Goble AJ, Elliott PC, et al. Mild depression predicts long-term mortality after acute myocardial infarction: a 25-year follow-up. Heart Lung Circ 2019; 28: 1812-1818.
23. Berg SK, Rasmussen TB, Thrysoee L, et al. Anxiety, depression and risk behaviour in cardiac patients. Findings from the national DenHeart survey. Eur Heart J 2017; 38: ehx502.2238.
24. Virani SS, Newby LK, Arnold SV, et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 2023; 148:e9-e119
25. Lapa ME, Swabe GM, Rollman BL, et al. Assessment of depression and adherence to guideline-directed medical therapies following percutaneous coronary intervention. JAMA Network Open 2022; 5: e2246317
26. Murphy BM, Le Grande M, Navaratnam H, et al. Are poor health behaviours in anxious and depressed cardiac patients explained by sociodemographic factors? Eur J Prev Cardiol 2013; 20: 995-1003.
27. Pająk A, Jankowski P, Kotseva K, et al. Depression, anxiety, and risk factor control in patients after hospitalization for coronary heart disease: the EUROASPIRE III Study. Eur J Prev Cardiol 2013; 20: 331-340.
28. Rao A, Zecchin R, Newton PJ, et al. The prevalence and impact of depression and anxiety in cardiac rehabilitation: a longitudinal cohort study. Eur J Prev Cardiol 2020; 27: 478-489.
29. Khandaker GM, Zuber V, Rees JMB, et al. Shared mechanisms between coronary heart disease and depression: findings from a large UK general population-based cohort. Mol Psychiatry 2020; 25: 1477-1486.
30. Sakamoto M, Suematsu Y, Yano Y, et al. Depression and anxiety are associated with physical performance in patients undergoing cardiac rehabilitation: a retrospective observational study. J Cardiovasc Dev Dis 2022; 9: 21.
31. Colquhoun DM, Bunker SJ, Clark DM, et al. Screening, referral and treatment for depression in patients with coronary heart disease: a consensus statement from the National Heart Foundation of Australia. Med J Aust 2013; 198: 483-484.
32. Thombs BD, Markham S, Rice DB, et al. Does depression screening in primary care improve mental health outcomes? BMJ 2021; 374: n1661.
33. Murphy BM, Higgins RO, Jackson AC, et al. Patients want to know about the ‘cardiac blues’. Aust Fam Physician 2015; 44: 826-832.
34. Murphy BM, Elliott PC, Higgins RO, et al. Anxiety and depression after coronary artery bypass graft surgery: most get better, some get worse. Eur J Cardiovasc Prev Rehabil 2008; 15: 434-440.
35. Hare DL, Toukhsati SR, Johansson P, et al. Depression and cardiovascular disease: a clinical review. Eur Heart J 2014; 35: 1365-1372.
36. Murphy BM, Higgins RO, Shand L, et al. Managing the cardiac blues in clinical practice: A survey of Australian cardiac health professionals. Br Cardiac Nursing 2016; 11: 222-228.
37. Murphy BM, Higgins RO, Shand L, et al. Improving health professionals’ self-efficacy to support patients’ emotional recovery after heart attack and heart surgery: The ‘cardiac blues project’. Eur J Cardiovas Nursing 2016; 16: 143-149.
38. Anderson L, Oldridge N, Thompson DR, et al. Exercise-based cardiac rehabilitation for coronary heart disease: cochrane systematic review and meta-analysis. J Am Coll Cardiol 2016; 67: 1-12.
39. De Gruyter E, Ford G and Stavreski B. Economic and social impact of increasing uptake of cardiac rehabilitation services –a cost benefit analysis. Heart Lung Circ 2016; 25: 175-183.
40. Driscoll A, Hinde S, Harrison A, et al. Estimating the health loss due to poor engagement with cardiac rehabilitation in Australia. Int J Cardiol 2020; 317: 7-12.
41. Wang L, Sun Y, Zhan J, et al. Effects of exercise therapy on anxiety and depression in patients with coronary heart disease: a meta-analysis of a randomized controlled study. Front Cardiovas Med 2021; 8: 730155.
42. Peterson JC, Charlson ME, Wells MT, et al. Depression, coronary artery disease, and physical activity: how much exercise is enough? Clin Ther 2014; 36: 1518-1530.
43. Blumenthal JA, Sherwood A, Babyak MA, et al. Exercise and pharmacological treatment of depressive symptoms in patients with coronary heart disease: results from the UPBEAT (Understanding the Prognostic Benefits of Exercise and Antidepressant Therapy) study. J Am Coll Cardiol 2012; 60: 1053-1063.
44. Richards SH, Anderson L, Jenkinson CE, et al. Psychological interventions for coronary heart disease: Cochrane systematic review and meta-analysis. Eur Prev J Cardiol 2018; 25: 247-259.
45. Ski CF, Jelinek M, Jackson AC, et al. Psychosocial interventions for patients with coronary heart disease and depression: A systematic review and meta-analysis. Eur J Cardiovasc Nurs 2016; 15: 305-316.
46. Reavell J, Hopkinson M, Clarkesmith D, et al. Effectiveness of cognitive behavioral therapy for depression and anxiety in patients with cardiovascular disease: a systematic review and meta-analysis. Psychosom Med 2018; 80: 742-753.
47. Li YN, Buys N, Ferguson S, et al. Effectiveness of cognitive behavioral therapy-based interventions on health outcomes in patients with coronary heart disease: A meta-analysis. World J Psychiatry 2021; 11: 1147-1166.
48. Tully PJ, Ang SY, Lee EJ, et al. Psychological and pharmacological interventions for depression in patients with coronary artery disease. Cochrane Database Syst Rev 2021; 12: Cd008012.
49. Murphy BM, Navaratnam HS, Le Grande MR, et al. Cognitive behavioral therapy enhances survival in cardiac patients aged under 60: 14-year outcomes of the Beating Heart Problems program trial. J Cardiopulm Rehabil Prev 2023; 43: 170-178.
50. Fernandes N, Prada L, Rosa MM, et al. The impact of SSRIs on mortality and cardiovascular events in patients with coronary artery disease and depression: systematic review and meta-analysis. Clin Res Cardiol 2021; 110: 183-193.
51. Celano CM, Daunis DJ, Lokko HN, et al. Anxiety disorders and cardiovascular disease. Curr Psychiatry Rep 2016; 18: 101.
52. Behlke LM, Lenze EJ, Carney RM. The cardiovascular effects of newer antidepressants in older adults, those with or at high risk for cardiovascular diseases. CNS Drugs 2020; 34: 1133-1147.
53. Huffman JC, Mastromauro CA, Beach SR, et al. Collaborative care for depression and anxiety disorders in patients with recent cardiac events: the Management of Sadness and Anxiety in Cardiology (MOSAIC) randomized clinical trial. JAMA Int Med 2014; 174: 927-935.
54. Ski CF, Cartledge S, Foldager D, et al. Integrated care in cardiovascular disease: a statement of the Association of Cardiovascular Nursing and Allied Professions of the European Society of Cardiology. Eur J Cardiovasc Nurs 2023; 22: e39-e46.
55. Hare DL, Stewart AGO, Driscoll A, et al. Screening, referral and treatment of depression by Australian cardiologists. Heart Lung Circ 2020; 29: 401-404.
56. Australian Bureau of Statistics. Patient Experiences 2021-22. 2023. Canberra.
57. Marin TS, Walsh S, May N, et al. Screening for depression and anxiety among patients with acute coronary syndrome in acute care settings: a scoping review. JBI Evid Synth 2020; 18: 1932-1969.
58. Brown M, Moore CA, MacGregor J, et al. Primary Care and Mental Health: Overview of Integrated Care Models. J Nurse Pract 2021; 17: 10-14.
59. Jackson AC, Le Grande MR, Higgins RO, et al. Psychosocial screening and assessment practice within cardiac rehabilitation: A survey of cardiac rehabilitation coordinators in Australia. Heart Lung Circ 2017; 26: 64-72.
60. Astley CM, Chew DP, Keech W, et al. The impact of cardiac rehabilitation and secondary prevention programs on 12-month clinical outcomes: a linked data analysis. Heart Lung Circ 2020; 29: 475-482.
61. Helmark C, Harrison A, Pedersen SS, et al. Systematic screening for anxiety and depression in cardiac rehabilitation – are we there yet? Int J Cardiol 2022; 352: 65-71.
62. Grace SL, Grewal K, Stewart DE. Factors affecting cardiac rehabilitation referral by physician specialty. J Cardiopulm Rehabil Prev 2008; 28: 248-252.