Intensive lipid-modifying therapy: why, when, who and how?
Because of issues related to the efficacy, safety and cost effectiveness of lipid-modifying drugs, physicians have a challenge to ensure these drugs are prescribed for the correct patient at the right time and in the correct manner. Patients have some responsibility to assist in this process, often in the face of an adverse lay media environment.
- Intensive lipid-modifying therapy is strongly indicated for all instances of secondary cardiovascular disease prevention alongside management of other conventional risk factors.
- Less intensive lipid-modifying therapy is indicated for primary cardiovascular prevention in selected patients with high cardiovascular risk.
- Low-density lipoprotein (LDL)-cholesterol targets are necessary and are generally attainable with appropriate therapy.
- Adverse events sometimes occur in patients receiving intensive lipid-modifying therapy, for a variety of reasons, and require careful and sensitive management.
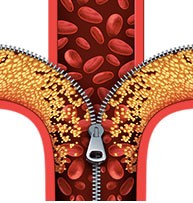
Picture credit: © Freshidea/stock.adobe.com
The past 30 years have witnessed the development of new lipid-modifying drugs that permit effective management of lipid abnormalities in most patients. These lipid-modifying drugs include:
- drugs that reduce cholesterol synthesis and thereby enhance low-density lipoprotein (LDL) receptor activity (statins)
- drugs that reduce cholesterol absorption (ezetimibe)
- drugs that inhibit the enzyme proprotein convertase subtilisin- kexin type 9 (PCSK9) and thereby enhance LDL receptor activity (evolocumab, alirocumab)
- drugs that interfere with RNA messaging and thereby inhibit synthesis of apolipoprotein B100 of LDL (mipomersen) or PCSK9 (inclisiran); these drugs are not currently available in Australia for general use.
This list is not exhaustive.
Efficacy of lipid-modifying therapy: why and when to use
Epidemiological studies have shown that LDL-cholesterol (LDL-C) is an important risk factor in the development of cardiovascular disease, whether this be a first event or a recurrent event. Controlled trials confirm the efficacy of statin therapy in reducing future cardiovascular (CV) risk and mortality. The lowest event rates are achieved in those groups achieving the lowest LDL-C levels. A well-justified mantra has arisen: ‘In regard to LDL-C, the lower the better’. Patients receiving lipid-modifying therapy should also follow diet and lifestyle advice with appropriate attention to other major risk factors such as hypertension, diabetes and cigarette smoking.
The Cholesterol Treatment Trialists’ Collaboration, in a 2005 report based on 14 statin trials, confirmed a significant reduction in CV events: a 21% reduction in major CV events for every 1 mmol/L reduction in LDL-C level over five years.1 As illustrated in Figure 1, patients with previous coronary heart disease (CHD) had about double the number of major CV events avoided over five years compared with those without previous CHD.
A later report based on 26 randomised trials explored whether more intensive statin therapy might be even more effective.2 More intensive statin therapy (40 to 80 mg atorvastatin or 10 to 20 mg rosuvastatin daily) compared with less intensive statin therapy (simvastatin 20 to 40 mg daily) produced an extra 15% reduction in major CV events. These findings suggest that reducing LDL-C by 2 to 3 mmol/L might reduce relative risk by around 40 to 50% overall. Reductions in LDL-C of this order can be achieved regularly in routine clinical practice.
Although the reduction in relative risk of an event is largely independent of baseline LDL-C, it is clear that patients in secondary prevention have a much higher absolute risk and hence will achieve more disease prevention from therapy (Figure 1). There is evidence that lipid-modifying therapy in primary prevention is effective, but it is much less cost-effective, and less-intensive therapy in this group is generally recommended only for those at high CVD risk.3 They include patients with LDL-C level greater than 5.5 mmol/L or those with lesser elevations in LDL-C who simultaneously manifest other major CVD risk factors. An increased coronary artery calcium score, when available, might also be justification for such therapy.
The role of nonstatin therapy has been the subject of renewed interest. Ezetimibe administered in a controlled trial to patients with a recent acute coronary syndrome, all of whom received statin plus other standard therapy, achieved a further 6% reduction in major CV events compared with placebo (Figure 2).4 This benefit is additional to that previously demonstrated with the use of a statin alone.1 Patients with a past history of coronary bypass surgery treated with ezetimibe achieved a larger (20%) reduction in major CV events.5
The general case for intensive lipid-modifying therapy in the context of secondary prevention is beyond doubt, but there are always safety considerations, which will now be addressed.
Safety of therapy
Every practitioner has witnessed a small proportion of patients with side effects when using statins. These include muscle symptoms, new-onset diabetes, liver dysfunction, central nervous system symptoms, drug–drug interactions or other nonspecific symptoms. Many prescribers and many patients seek to avoid statin therapy because of the presence of or concern about possible statin-associated side effects, whether causally related or not. Fearmongering on television, the Internet and in other lay media portrays adverse events out of perspective. Such reporting is unbalanced, highlights side effects while ignoring positive benefits, and results in our patients perceiving the wrong educational message.
A question arises – why do controlled trials with statins show broadly similar rates of adverse events in patients on active versus placebo treatments? Firstly, some patients have previously experienced side effects with statins or have comorbidity and are deliberately excluded from enrolment. Secondly, the trials are actually informing us that many adverse events are placebo-related. Thirdly, information on low frequency adverse events cannot be accurately determined unless sought by formal and specific testing.
Although more severe muscle problems will not be discussed here, muscle symptoms most commonly manifest as generalised myalgia with little or no change in serum muscle enzyme levels. This may occur in perhaps 10% of statin-treated patients.6 In a double-blind crossover study involving 472 patients, all with a prior history of statin-associated muscle symptoms, 44% developed muscle symptoms with atorvastatin but not with placebo, 28% did so with placebo treatment but not with atorvastatin, 10% did so on both atorvastatin and placebo, and 18% had no symptoms with either treatment.7
Statin-associated muscle symptoms, whether causally related or a placebo effect, require ongoing management in affected patients. Such management will not always be evidence-based. Hypothyroidism and vitamin D deficiency should be excluded, although there is little evidence that a vitamin D supplement will reduce symptoms. Drug–drug interactions need to be considered. There is no convincing evidence that a coenzyme Q10 supplement will assist beyond any placebo effect, but that may be enough in a few instances. A switch to another statin at a low dose may be helpful, even a move to intermittent dosing two to three times per week. A low-dose statin may be combined with daily ezetimibe. Sometimes a totally nonstatin approach will be necessary, such as ezetimibe alone or in combination with fenofibrate. Some of these approaches were discussed in detail in a previous article in Cardiology Today.8
Perhaps up to 20% of patients will develop new-onset diabetes on a statin, supposedly on the more potent statins.9 A large study with rosuvastatin found that essentially all of this risk occurred among those with baseline evidence of impaired fasting glucose (serum glucose level greater than 5.5 mmol/L). Reassuringly, the cardiovascular and mortality benefits with rosuvastatin were similar in those who did or did not develop new-onset diabetes.10
Managing side effects, placebo-induced or otherwise, requires considerable skill and rapport with patients. But we need to stress to patients that the benefits of lipid-modifying therapy are proven in those at high CV risk, and these benefits heavily outweigh the risk of side effects. But if side effects ultimately impair quality of life in any major way, lipid-modifying therapy may need to be suspended until new options become available (see below).
Who and how to treat
Based on the evidence discussed above, intensive lipid-modifying therapy is essential in all instances of secondary CV disease prevention. Less intensive therapy is desirable for primary prevention in patients at high CV risk, provided they have no contraindications. Patients with heterozygous familial hypercholesterolaemia are a unique group at high CV risk, whether they are in a secondary prevention category or not, and deserve more intensive lipid-modifying therapy in relevant cases.
The LDL-C target in secondary prevention is less than 1.8 mmol/L, although recent trial evidence suggests it could be set somewhat lower. Without debating this point, it would be helpful if many more of our patients achieved the current target. The target in primary prevention is less than 2.0 mmol/L. There is no biological reason that the target in primary prevention is different. It is just that these patients are at lower absolute risk and treatment is less cost effective, but is still justified in relevant high CV risk cases. Arbitrary targets exist for HDL-C and triglycerides, but these are not based on similarly firm evidence.
Intensive lipid-modifying therapy means using higher doses of potent statins. In patients with an acute coronary syndrome this is usually atorvastatin 40 or 80 mg daily. At follow up, clinicians may find such patients are not taking intensive lipid-modifying therapy because of side effects or other reasons. We should urge patients to return to this therapy if possible. Patients who have not reached the target LDL-C level may need further medication adjustment.
In more chronic care situations, lipid-modifying therapy may start at a lower dose of statin, but with a genuine need to uptitrate in doubling doses if the LDL-C level does not reach target values. Some patients on high-dose statin (or some unable to tolerate a high dose) will benefit from supplementary ezetimibe. A convenient single tablet of atorvastatin combined with ezetimibe is now available.
In practice, there is little or no risk of the LDL-C level falling too low on conventional therapy. But if the LDL-C level on high-dose statin is found to be under 1.0 mmol/L, the dose can be downtitrated. The big issue in practice is that too many patients on treatment have not achieved or nearly achieved target values.
Patients may not persist with therapy
In the treatment of chronic asymptomatic disease (e.g. hypercholesterolaemia or hypertension), patients may not persist with their medications long term.11 Examination of dispensed prescriptions for statin drugs initiated in almost 800,000 patients in the period 2006 to 2010 on the PBS revealed that 23% did not collect the first repeat prescription at one month and 47% had stopped collecting their repeat prescriptions at 12 months (Figure 3). Re-examination of persistence in more recent years has found essentially no change in this situation.
Poor persistence cannot simply be attributed to widespread side effects, but there may be a significant contribution of fear from the lay media, as discussed above. In reality, this is a sociological problem where long-term persistence with therapy may have no immediate or tangible benefit. This problem can be assisted by increased practitioner support and better patient education. Patients need to know that their lipid problem has been controlled, not cured. Cessation of therapy will lead to a rapid rise in LDL-C level with gradual loss in the benefit already achieved.
The future
The PCSK9 inhibitors, evolocumab and alirocumab, are able to reduce LDL-C level by 50 to 60%. Evolocumab was administered over a median period of 2.2 years in a very large controlled trial to patients with a history of CHD, all of whom received statin plus other standard therapy. They achieved a further 15% reduction in major CV events, representing a number needed to treat of 50 over 36 months to prevent one major CV event. Mean LDL-C level on evolocumab was 0.78 mmol/L, with no apparent safety concerns (Figure 4).12
This therapy requires a fortnightly subcutaneous self-injection by the patient. Apart from occasional injection-site reactions, this treatment has proven to be generally well tolerated, even by patients who could not tolerate other lipid-modifying drugs. Being a fully human monoclonal antibody, these PCSK9 inhibitors are expensive, and cost constraints will limit their ultimate availability on the PBS. PCSK9 inhibitors will not replace successful conventional lipid-modifying therapy. More information on these drugs may be found in a recent issue of Medicine Today.13
PCSK9 activity may also be reduced through administration of a chemically synthesised small interfering RNA designed to silence messenger RNA. Known as inclisiran, it is administered by subcutaneous injection and has produced major reductions in LDL-C level. It may only need to be administered at intervals of three months or longer.14 This product will require further long-term evaluation and may not reach the clinic for some years.
Conclusion
Intensive lipid-modifying therapy is strongly indicated in secondary CV prevention, alongside management of other conventional risk factors. Less-intensive therapy is Indicated in selected instances of high CV risk primary prevention. LDL-C targets are necessary and generally attainable with appropriate therapy. Adverse events sometimes occur and require careful and sensitive management.
References
- Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005; 366: 1267-1278.
- Cholesterol Treatment Trialists’ Collaboration. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010; 376: 1670-1681.
- US Preventive Services Task Force. Statin use for the primary prevention of cardiovascular disease in adults. JAMA 2016; 316: 1997-2007.
- Cannon CP, Blazing MA, Giugliano RP, et al; IMPROVE-IT Investigators. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med 2015; 372: 2387-2397.
- Eisen A, Cannon CP, Blazing MA, et al. The benefit of adding ezetimibe to statin therapy in patients with prior coronary artery graft surgery and acute coronary syndrome in the IMPROVE-IT trial. Eur Heart J 2016; 37: 3576-3584.
- Thompson PD, Panza G, Zaleski A, Taylor B. Statin-associated side effects. J Am Coll Cardiol 2016; 67: 2395-2410.
- Nissen SE, Stroes E, Dent-Acosta RE, et al. Efficacy and tolerability of evolocumab vs ezetimibe in patients with muscle-related statin intolerance: the Gauss-3 randomized clinical trial. JAMA 2016; 315: 1580-1590.
- Simons LA. Challenging cases in lipid and CVD prevention. A retrospective and an update. Cardiol Today 2014; 4(3): 29-33.
- Sattar N, Preiss D, Murray HM, et al. Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet 2010; 375: 735-742.
- Ridker PM, Pradhan A, MacFadyen JG, et al. Cardiovascular benefits and diabetes risks of statin therapy in primary prevention. Lancet 2012; 380: 565-571.
- Simons LA, Ortiz M, Calcino G. Long term persistence with statin therapy – experience in Australia 2006-2010. Aust Fam Physician 2011; 40: 319-322.
- Sabatine MS, Giugliano RP, Keech AC, et al; FOURIER Steering Committee and Investigators. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med 2017; 376: 1713-1722.
- Simons LA. Alirocumab and evolocumab. A new era in cholesterol control. Med Today 2016; 17(10): 51-53.
- Ray KK, Landmesser U, Leiter LA. Inclisiran in patients with high cardiovascular risk with elevated LDL cholesterol. N Engl J Med 2017; 376: 1430-1440.