Abdominal aortic aneurysms. Part 2: Surgery and postoperative care
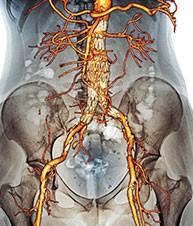
Endovascular stent graft technology has become the first-line and default surgical treatment of abdominal aortic aneurysms by many vascular surgeons throughout Australia and internationally. This second part of a two-part article discusses the surgical treatments available for abdominal aortic aneurysm repair, postoperative care and long-term follow up.
- Repair of an abdominal aortic aneurysm (AAA) is considered when its size reaches 5.5 cm in men or 5.0 cm in women.
- Endovascular aneurysm repair (EVAR) is less invasive than open surgery; however, there are anatomical limitations to its application.
- Open surgical repair of a AAA is signi cantly more invasive and carries more operative and short-term risk than EVAR; however, it can be used to treat a wider range of AAAs and has long-term data supporting its use.
- Follow up of postoperative AAA repair should be lifelong, irrespective of surgical technique.
- EVAR requires stringent follow up involving lifelong imaging surveillance because stent grafts can fail at any stage postoperatively. Secondary intervention is required in up to 26% of patients at 15 years after EVAR.
- Endoleaks from EVAR can be life-threatening and affected patients should be referred to a vascular surgeon immediately.
Picture credit: © Zephyr/SPL
Abdominal aortic aneurysms (AAAs) are considered for treatment when their size reaches 5.5 cm in men or 5.0 cm in women. In recent years, there have been significant advances in the treatment of AAAs, with minimally invasive endovascular techniques becoming the primary modality of surgical treatment, superseding the traditional open-surgery technique. Initially an option only for patients that were deemed unfit for open surgery, endovascular stent graft technology has progressed at an exponential rate such that it now has become the first-line option and default choice for the surgical treatment of AAAs by many vascular surgeons throughout Australia and internationally.1
This article discusses the surgical options available for AAA repair as well as postoperative care, including what to be mindful of in the new endovascular era. The assessment, surveillance and indications for repair of AAA are discussed in part 1 in the October 2016 issue of Cardiology Today.2
Open AAA surgery
There have been multiple advances in open surgical repair of AAAs since the 1950s; however, the basic premise has remained unchanged. Open surgical repair involves replacing the aneurysmal segment of aorta with a prosthetic graft through an invasive transperitoneal or, less commonly, retroperitoneal approach (Figures 1a and b).
Depending on the location of the aneurysm, a tube graft or bifurcated graft can be used. Sometimes during the surgery, temporary interruption of blood supply to the kidneys and visceral organs is required.
Improvements in surgical techniques, graft construction, general anaesthesia and postoperative intensive care have led to reduced morbidity and mortality from open surgery.
Advantages of open surgery
Long-term data demonstrate durability of and reduced rupture rate after open surgical AAA repair, and there are no anatomical limitations for performing an open AAA repair.3 Compared with endovascular aneurysm repair (EVAR), postoperative follow up of open AAA repair is not as intensive or onerous.
Disadvantages of open surgery
The main disadvantages of open AAA surgery are related to the procedure being a major operation and effects on surrounding anatomical structures.
Major surgery
Open AAA repair is major surgery and compared with EVAR, carries a significantly higher perioperative mortality (3.7% vs 1.3%) and morbidity.4,5 The procedure cannot be performed under local or regional anaesthesia, and patients with significant cardiovascular and respiratory comorbidities may not have the physiological reserve needed to survive open AAA repair. Recovery from an open AAA repair is significantly longer than recovery following EVAR.6
Effects on surrounding structures
During open surgery for aneurysms involving the renal and visceral segment of the aorta, interruption of blood supply to the kidneys and visceral organs may be required, leading to higher rates of perioperative morbidity, including renal failure, visceral ischaemia and paraplegia, and increased mortality.7 Compared with EVAR, open AAA repair in men results in a higher rate of sexual dysfunction, which can occur in up to 80% of patients due to nerve damage and ischaemia.8
Endovascular aneurysm repair
EVAR involves excluding the aneurysm from the circulation with a covered stent graft (Figures 2a and b). This is routinely performed via both femoral arteries with access in the groins.
There have been significant advances in stent grafts during the past two decades, leading to more AAAs being suitable for EVAR. Treatment of complex juxtarenal, suprarenal and thoraco-abdominal aneurysms, involving visceral and renal segments of the aorta, was previously exclusively the domain of open surgery. Many of these can now be treated with EVAR using custom-made grafts with adjunctive endovascular techniques to stent the renal or visceral arteries through fenestrations or branches.9
Advantages of an endovascular approach
As previously mentioned, EVAR has a significantly lower perioperative morbidity and mortality compared with open surgery.5,10 However, data have suggested that this mortality advantage of EVAR over open surgery does not persist beyond two years.11,12
EVAR can be performed under local or regional anaesthesia, mitigating the risks of general anaesthesia. Postoperative recovery is faster and the rate of discharge home with premorbid function is higher compared with open surgery.6 For these reasons, EVAR can be offered to some patients who may not be suitable for open surgery due to comorbidities and unacceptable surgical/anaesthetic risk.
Disadvantages of an endovascular approach
A chief disadvantage of the endovascular approach is that it cannot be performed in all patients with a AAA. There are multiple anatomical constraints that can exclude EVAR as a treatment option; these are described later in this article.
Another disadvantage is the need for life-long imaging surveillance, which includes exposure to radiation, to monitor for graft complications and failures. Late secondary rupture following EVAR is seen in up to 5% of patients,12 and the need for secondary interventions is significantly higher in patients following EVAR compared with open repair (26% vs 12% over 15 years).11,13
EVAR is associated with exposure to radiation from x-ray and the use of iodinated contrast, which can be an initial concern, and the financial costs of stent grafts can be significant to the healthcare system.
A comparison of advantages and disadvantages of EVAR and open surgery are summarised in Table 1.11–13
Selecting the best mode of surgery
The decision to intervene has been discussed in part 1 of this article.2 Selecting the best mode of surgical intervention for the patient is complex, with multiple factors to consider. These can largely be separated into patient factors and aneurysm factors.
Patient factors
Age
Age is an important factor, especially when considering the natural history of the disease. Younger patients with a longer life expectancy may favour open AAA repair over EVAR due to the proven durability of replacing the aneurysmal segment.
Comorbidities
If the patient has significant cardiovascular or respiratory compromise, the patient may not be fit for general anaesthesia or open AAA repair and EVAR may be the only surgical option. Renal failure may influence the decision against EVAR because of the amount of potentially nephrotoxic iodinated contrast used.
AAAs that occur in patients with a connective tissue disorder have compromised structural integrity of the aortic wall and EVAR is generally not recommended in this cohort of patients.14
Other factors
Lifestyle and occupational factors that may preclude a patient from having intensive imaging surveillance or the higher risk of potential secondary interventions may influence the decision against EVAR.
Aneurysm factors
Site and anatomy
Aneurysmal involvement of the renal and visceral aorta excludes conventional EVAR, and complex fenestrated or branched stent grafts or open AAA repair remain the only options. EVAR is difficult when the segment immediately below the renal arteries (the infrarenal neck) is highly angulated.
Inadequate sealing zone
The sealing zone for EVAR is the zone of healthy, non-aneurysmal aortic or arterial vessel wall into which the stent graft can be fixed and sealed, excluding the aneurysm from the circulation. This sealing zone applies to both the proximal (usually the segment below the renal arteries) and distal portions of the graft (usually the common iliac arteries). If there is an insufficient seal zone length (required length varies depending on the type of stent graft), conventional EVAR may not be possible. In this situation, complex fenestrated or branched stent grafts or open AAA repair are the only options.
Thrombosis and calcification
Significant juxtarenal intraluminal thrombus or calcification within the aorta can preclude EVAR because there is a risk of poor seal and also distal embolisation into the renal arteries.
Access vessels
The access vessels for EVAR are the iliac and femoral arteries. There is a minimum diameter of these vessels that is required for EVAR. Excessive tortuosity and calcification of these vessels can also preclude suitability for EVAR.
Postoperative care
Inpatient care
Immediate postoperative care within the hospital is tailored to the patient and based on the type of surgical repair. Generally EVAR patients have a shorter recovery time and inpatient stay compared with patients that have had open AAA repair. There is a greater chance that patients will need a period of inpatient rehabilitation if they have had an open AAA repair. Depending on the treating institution, the first postoperative radiological scan for EVAR can be performed as an inpatient.
Outpatient care
Once the patient has been discharged, the following general postoperative measures should be advised.
- Avoid heavy lifting for four to six weeks, particularly after an open AAA repair.
- Avoid driving until feeling safe to perform an emergency brake.
- Mobilise early, with a gradual increase in physical activity.
Complications
Graft infection
Graft infection can occur with both open AAA repair and EVAR. It can present insidiously with a myriad of symptoms but fever, general malaise and abdominal or back pain are the most common. Infection is a serious and potentially life-threatening issue and immediate referral to a specialist vascular surgeon is warranted.15
Infection of the graft after an open AAA repair can affect pre- existing groin wounds, if a bifurcated graft has been joined to the femoral arteries. If not involving the groin, infection of an open graft or endovascular stent graft is usually suspected on clinical history alone, as there are rarely obvious clinical signs. This can be confirmed on imaging and microbiological tests.
Junctional aneurysm
After open surgery, junctional aneurysms or false aneurysms can result from breakdown of the anastomoses. These can present as pulsatile masses in the groin or as an incidental finding on surveillance imaging. They can also be manifestations of an infective process.16
Endoleak
An endoleak is a complication specific to EVAR, in which the stent graft fails to exclude the AAA from the circulation, resulting in arterial flow into the AAA sac (outside the graft stent). This can lead to ongoing expansion of the AAA sac and, potentially, rupture and death.
Endoleaks can occur due to:
- an inadequate seal resulting in leaking at the graft stent end into the aneurysmal sac (type I, most serious)
- bleeding directly into the aneurysm sac from lumbar arteries or the inferior mesenteric artery (type II)
- graft material defects, stent migration or stent fatigue (type III).17
Some endoleaks require urgent intervention, whereas others can be safely monitored. Type I endoleaks are the most serious, and affected patients should be referred to see a specialist vascular surgeon immediately. All patients with an endoleak should be referred to a vascular surgeon for assessment.
Other complications
Other complications common to both open and endovascular repair include graft migration and thrombosis. Patients with wound or groin infections should be referred back to the vascular surgeon as a matter of urgency.
Early in the postoperative EVAR phase, patients can have a systemic response to the stent graft, which can manifest as elevated temperature and raised inflammatory markers. A thorough infection screen is essential to exclude sepsis; however, most of these inflammatory responses can be managed conservatively provided infection has been excluded.
Postoperative surveillance
Recommended surveillance following EVAR
Postoperative imaging surveillance is of utmost importance following EVAR because there are problems that can be detected despite the patient remaining asymptomatic.18 Complications that may be identified on imaging include endoleak, graft infection, graft migration and thrombosis.
Life-long imaging surveillance by ultrasound scanning or CT angiography is recommended. Although a specialist vascular surgeon usually follows up patients who have had an EVAR, the GP can facilitate surveillance imaging if the patient has been lost to follow up.
The intervals for surveillance imaging and modality of imaging will differ among institutions and surgeons; however, a suggested post-EVAR surveillance plan involves imaging at six weeks, three months, six months, 12 months and annually thereafter.
Recommended surveillance following open repair
A suggested postoperative review plan involves clinical review at six weeks, three months, six months, 12 months and annually thereafter. Postoperative imaging is not routine practice after open AAA repair.
Role of the GP
The role of the GP is important in the decision-making, postoperative recovery and long-term surveillance of patients considering or undergoing AAA surgery. Knowledge of the different surgical options and the merits of both open AAA repair and EVAR are important in counselling and informing patients. It is important that the GP has a thorough knowledge of the longer-term issues and implications especially for EVAR because patients can be lost to follow up in the hospital setting.
Conclusion
Surgery to repair AAAs has changed significantly in recent times; EVAR has overtaken open surgical repair as the default choice in Australia. A thorough knowledge of surgical procedures including factors affecting choice of procedure, limitations, complications and long-term follow up are vital for GPs managing patients with this condition.
References
- Albuquerque FC Jr, Tonnessen BH, Noll RE Jr, et al. Paradigm shifts in the treatment of abdominal aortic aneurysm: trends in 721 patients between 1996 and 2008. J Vasc Surg 2010; 51: 1348-1352.
- Goh D, Chuen J. Abdominal aortic aneurysms Part 1: Assessment and surveillance. Cardiology Today 2016; 6(4): 20-23.
- Conrad MF, Crawford RS, Pedraza JD, et al. Endovascular versus open repair of abdominal aortic aneurysm in 15-years’ follow-up of the UK endovascular aneurysm repair trial 1 (EVAR trial 1): a randomised controlled trial. J Vasc Surg 2007; 46: 669-675.
- Zwolak RM, Sidawy AN, Greenberg RK, et al. Lifeline registry of endovascular aneurysm repair: open repair surgical controls in clinical trials. J Vasc Surg 2008; 48: 511-518.
- Malas M, Arhuidese I, Qazi U, et al. Perioperative mortality following repair of abdominal aortic aneurysms: application of real a randomized controlled trial to real-world practice using a validated nationwide data set. JAMA Surg 2014; 149: 1260-1265.
- Arko FR, Hill BB, Reeves TR, et al. Early and late functional outcome assessments following endovascular and open aneurysm repair. J Endovasc Ther 2003; 10: 2-9.
- Nathan DP, Brinster CJ, Woo EY, et al. Predictors of early and late mortality following open extent IV thoracoabdominal aortic aneurysm repair in a large contemporary single-center experience. J Vasc Surg 2011; 53: 299-306.
- Lee ES, Kor DJ, Kuskowski MA, Santilli SM. Incidence of erectile dysfunction after open abdominal aortic aneurysm repair. Ann Vasc Surg 2000; 14: 13-19.
- Franks SC, Sutton AJ, Bown MJ, Sayers RD. Systematic review and meta-analysis of 12 years of endovascular abdominal aortic aneurysm repair. Eur J Vasc Endovasc Surg 2007; 33: 154-171.
- EVAR trial participants. Endovascular aneurysm repair versus open repair in patients with abdominal aortic aneurysm (EVAR trial 1): randomised controlled trial. Lancet 2005; 365: 2179-2186.
- Patel R, Sweeting MJ, Powell JT, Greenhalgh RM; EVAR trial investigators. Endovascular versus open repair of abdominal aortic aneurysm in 15-years follow-up of the UK endovascular aneurysm repair trial 1 (EVAR trial 1): a randomised controlled trial. Lancet 2016; 388: 2366-2374.
- Powell JT. Prophylactic abdominal aortic aneurysm repair? Open repair brings early pain but later gain. Eur J Vasc Endovasc Surg 2016; 52: 719-720.
- Lederle FA, Freischlag JA, Kyriakides TC, et al. Long-term comparison of endovascular and open repair of abdominal aortic aneurysm. N Engl J Med 2012; 367: 1988-1997.
- Svensson LG, Kouchoukos NT, Miller DC, et al. Expert consensus document on the treatment of descending thoracic aortic disease using endovascular stent-grafts. Ann Thor Surg 2008; 85: S1-S41.
- Laser A, Baker N, Rectenwald J, et al. Graft infection after endovascular abdominal aortic aneurysm repair. J Vasc Surg 2011; 54: 58-63.
- Edwards JM, Teefey SA, Zierler RE, Kohler TR. Intraabdominal paraanastomotic aneurysms after aortic bypass grafting. J Vasc Surg 1992; 15: 344-350 and 351-353.
- Chuter TA, Faruqi RM, Sawhney R, et al. Endoleak after endovascular repair of abdominal aortic aneurysm. J Vasc Surg 2001; 34: 98-105.
- van Marrewijk C, Buth J, Harris PL, et al. Significance of endoleaks after endovascular repair of abdominal aortic aneurysms: the EUROSTAR experience. J Vasc Surg 2002; 35: 461-473.