Diagnosing chest pain
Articles in this section are inspired by, but not based on, real cases to illustrate the importance of knowledge about ECGs in relation to clinical situations in general practice. Management is not discussed in detail.
- Chest pain is common, but if an acute cardiac cause or other emergency cannot be excluded then the patient should be assumed to have these until proven otherwise.
- In acute ST elevation myocardial infarction (STEMI), the first changes are hyperacute T waves, followed by ST elevation within the hour; T waves begin to invert at 12 to 24 hours; the baseline returns to normal at 24 hours, but T wave inversion lasts days to months.
- Pathological Q waves are seen in the first few hours, evolve over days and are permanent.
- Normal Q waves typically occur in the trace from the left-sided leads (chest leads V5 and V6 and limb leads 1 and aVL).
Zhang is a 43-year-old man unknown to your medical practice. He comes in unexpectedly, saying his work colleagues told him to see a doctor. He tells you that he is feeling ‘nonspecifically’ unwell and has had central and left-sided chest heaviness for the past 45 minutes. This came on over a minute or so while he was sitting at work and has been constant, not changing with walking or breathing. He is not short of breath.
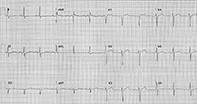
You assess Zhang urgently. He looks pale, anxious and clammy. He is moderately overweight and is holding his chest with both hands. His blood pressure is 145/95 mmHg and pulse rate is 90 beats per minute and regular. His oxygen saturation is 98% on room air. Cardiac and respiratory auscultation findings are normal. He tells you he has not seen a doctor for years, has no known medical problems and takes no medications. He smokes five cigarettes daily and has about three standard drinks of alcohol (30 g) daily on weekends. You immediately organise an ECG recording (Figure).
Q1. What does this ECG show?
The ECG shows:
- heart rate of 72 beats per minute, in sinus rhythm
- the following intervals – PR157 ms; QRS 122 ms; QT 422 ms; and QTc 446 ms
- ST elevation in the anteroseptal leads of about 1 mm (0.1 mV)
- nonspecific T wave changes.
Q2. What should be done while the ECG is being arranged?
The GP should arrange for someone to telephone the national emergency number (000) as soon as it is obvious the patient’s chest discomfort could have a cardiac origin, and notify the operator of this possibility so they can arrange a coronary care ambulance. The patient should be given aspirin 300 mg (unless allergic to this) with a little milk or water. They should also be given a glyceryl trinitrate wafer or spray sublingually, initially one wafer or two spray presses. Oxygen is not recommended if the oxygen saturation is normal. The patient should be asked to nominate a contact person, as they must to go to hospital urgently in case the chest discomfort is related to the heart. A further history should be taken regarding family health and any indicators of muscular injury or a recent viral infection.
Q3. What is the differential diagnosis?
The differential diagnosis in Zhang’s case includes:
- cardiac causes of chest discomfort, such as coronary ischaemia, pericarditis, myocarditis (including COVID-19 myocarditis) and Takotsubo cardiomyopathy
- respiratory causes of chest discomfort, such as a pulmonary embolus; less likely respiratory causes include pleurisy (the discomfort of pleurisy is typically sharp and varies with breathing), severe bronchitis or pneumonia (which is usually accompanied by a cough and abnormal findings on auscultation) and pneumothorax (where the discomfort is associated with breathing and shortness of breath)
- musculoskeletal discomfort, such as costochondritis and muscular strain
- gastrointestinal discomfort, such as oesophagitis, oesophageal spasm and incarcerated sliding paraoesophageal hernia (but Zhang has no history of recent activities to provoke this)
- aortic disease, such as an aneurysm leak or dissection (pain is usually described as searing and radiating to the back).
Q4. What is the definition of acute ST elevation myocardial infarction?
Acute ST elevation myocardial infarction (STEMI) is defined as an ST elevation at the J point (junction between the termination of the QRS complex and the beginning of the ST segment) in two contiguous leads that is:
- at least 1 mm in all leads other than V2 and V3
- greater than or equal to sex- and age-specific values in leads V2 and V3: 1.5 mm (women), 2 mm (men aged 40 years or over) and 2.5 mm (men aged under 40 years).1
The ST elevation usually has a convex (‘tombstone’) shape, in contrast to the concave elevation seen in pericarditis.
There may also be reciprocal ST depression in leads V1, V2, V3 and V4, which suggests posterior myocardial ischaemia or infarction. New left bundle branch block is treated as STEMI in the appropriate clinical context because it is not possible to observe the typical ECG changes of myocardial infarction in its presence.
Zhang may be developing the earliest signs of ST elevation in the anteroseptal leads V1 to V4.
Q5. How do ECG changes evolve in patients with acute STEMI?
In patients undergoing an acute STEMI, the first ECG changes are hyperacute T waves, which signify the beginning of myocardial ischaemia. ST elevation follows within an hour and denotes myocardial damage. If reperfusion occurs at this stage (spontaneously or through primary angioplasty or thrombolysis), the ST elevation should fall by 50% within the next 1.5 hours. T waves begin to invert at 12 to 24 hours, designating the absence of ongoing ischaemia. The ST segment returns to baseline by 24 hours, but T wave inversion may persist for days to months. The pathological Q wave, if present, appears in the first few hours, evolves over days and is permanent. If it is not present, the ECG may even return to a normal appearance.
The signs of an old myocardial infarction are pathological Q waves or poor R wave progression across the chest leads (loss of normal increasing R wave size, which should be larger than the S wave by lead V4). Poor R wave progression is not specific to an old anterior myocardial infarction and may also be associated with left or right ventricular hypertrophy, dilated cardiomyopathy, incorrect lead placement or a variation of normal. If pathological, it is due to loss of anterior forces.
A persistent elevation of the ST segment suggests a complication of an old myocardial infarction, a left ventricular aneurysm.
Q6. How do ECG findings correlate with affected regions of the heart?
In patients with myocardial infarction, the affected regions of the heart generally correspond to changes in the trace from the ECG leads as follows:
- septal region – leads V1 and V2
- anterior region – leads I, V3 and V4 and perhaps reciprocal changes in leads III and aVF
- lateral region – leads V5 and V6
- anteroseptal region – leads V1 to V4
- anterolateral region – leads I, aVL and V3 to V6
- inferior region – leads II, III and aVF
- posterior region – ST depression in leads V1 and V2 in conjunction with tall R waves in these leads
- extensive anterior region – leads V1 to V6 plus aVL
- high anterolateral region – leads I and aVL
- an extensive anterior myocardial infarction can manifest as new left bundle branch block.
Because of variation in coronary artery anatomy, the occluded artery may differ from the above patterns.2
Q7. What are Q waves?
Q waves are any negative deflection that occurs before the commencement of the R wave on an ECG trace. It reflects the left to right depolarisation of the interatrial septum. Q waves are classed as nonpathological (‘normal’) or pathological.
Normal Q waves typically occur in the traces from the left-sided leads: chest leads V5 and V6 and limb leads l and aVL. Normal Q waves, unlike pathological Q waves, are not seen in the right-sided leads (V1, V2 and V3) unless there is dextrocardia. Q waves may also be normal in leads III and aVR if up to 2 mm in depth and under a quarter of the depth of the QRS complex; they are also typically shallow. There should always be small Q waves in leads V5 and V6, and their absence suggests a conduction defect, typically left bundle branch block.
Pathological Q waves are at least 1 mm wide, with depth 2 mm or more or a quarter of the depth of the QRS complex or more. They may also evolve over hours to days after an acute myocardial infarction. Hence, pathological Q waves are a marker for a recent or longstanding myocardial infarction. They may also be seen in the presence of cardiomyopathy, especially hypertrophic obstructive cardiomyopathy, dextrocardia or cardiac rotation and incorrect lead placement.
Outcome
Zhang’s chest discomfort eases after administration of glyceryl trinitrate spray. His observations remain stable, and his ECG appears unchanged when the paramedic repeats the recording 15 minutes later. Zhang is treated as if he has acute myocardial ischaemia and transferred to a hospital that has a coronary catheter laboratory. His ECG continues to remain unchanged and his blood test results, especially his troponin level, remain normal over the next six hours. He is discharged home with a diagnosis of atypical chest pain and advised to follow up with his GP. CT